| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website https://www.theijcp.org |
Original Article
Volume 13, Number 3, December 2024, pages 86-95
Weaning From Mechanical Ventilation in Preterm Newborns: Ventilatory Profile and the Construction of an Extubation Protocol
Jhennif Sabrina da Silvaa, b, Valeria Emiliane Lopes Mourac, Ana Cristina de Oliveira Costad , Ana Carolina Gomide Micheletti Gomide Nogueira de Sae, f
, Isabella Diniz Fariag, h, i, j
aMultiprofessional Residency Program, Health of the Municipal Government of Contagem, Contagem, Brazil
bPhysiotherapy Department, Maternal and Child Center of the Municipal Government of Contagem, Contagem, Minas Gerais, Brazil
cNeonatal and Pediatric Intensive Therapy, Physiotherapy Department, Maternal and Child Center of the Municipal Government of Contagem, Contagem, Minas Gerais, Brazil
dResearch Group on Health Policies and Social Protection, Rene Rachou Institute, Oswaldo Cruz Foundation, Belo Horizonte, Minas Gerais, Brazil
eDepartment of Maternal and Child and Public Health, Federal University of Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
fPostgraduate Program, School of Nursing, Federal University of Minas Gerais, Minas Gerais, Brazil
gThe Brazilian Company of Hospital Services (EBSERH), UFMG Clinics Hospital, Belo Horizonte, Minas Gerais, Brazil
hPhysiotherapy Department, Multiprofessional Health Residency Program of the Municipal Government of Contagem, Contagem, Minas Gerais, Brazil
iSpecialized Care Center Iria Diniz, Contagem, MG 32010-000, Brazil
jCorresponding Author: Isabella Diniz Faria, Specialized Care Center Iria Diniz, Contagem, MG 32010-000, Brazil
Manuscript submitted May 21, 2024, accepted July 8, 2024, published online September 16, 2024
Short title: Weaning From Mechanical Ventilation in PTNBs
doi: https://doi.org/10.14740/ijcp515
| Abstract | ▴Top |
Background: Weaning from invasive mechanical ventilation and the ideal time for extubation of preterm newborns (PTNBs) should be performed early. However, the ideal time to perform them is still a challenge in neonatal intensive care unit (NICU). The aim of the study was to present the ventilatory profile of premature infants submitted to invasive mechanical ventilation, assess the extubation failure rate and the elaboration of an extubation protocol.
Methods: This was a descriptive cross-sectional study carried out in an NICU with PTNBs who underwent invasive mechanical ventilation for a period longer than 24 h.
Results: Twenty-seven PTNBs participated in this study, from which 43 extubation events originated. The overall extubation failure rate observed in the study was 23.3%, being higher among PTNBs younger than 28 weeks (50%). Regarding the failure rates according to birth weight ranges, extremely low weight PTNBs (less than 1,000 g) had the highest rates, followed by very low weight PTNBs (1,000 g to 1,499 g), with rates of 33.3% and 21.4%, respectively.
Conclusions: Knowing the ventilatory profile of PTNBs and the risk factors associated with extubation failure facilitates the weaning process and increases the chance of successful extubation.
Keywords: Mechanical ventilation; Weaning from mechanical respirators; Extubation; Protocols; Preterm newborns
| Introduction | ▴Top |
Invasive mechanical ventilation (IMV) aims to provide adequate ventilation and oxygenation, being an extremely important support in the treatment of respiratory complications in preterm newborns (PTNBs). According to the World Health Organization, babies with a gestational age at birth (GA) of less than 37 weeks are considered PTNBs [1]. The literature documents that it is common for PTNBs to develop respiratory distress, due to the immaturity of the lung structure, inefficient muscle function, surfactant deficiency, increased airway resistance and high rib cage compliance [1]. These factors contribute to the dependence of PTNBs on the use of IMV [2, 3].
The prolonged use of IMV has a direct impact on hospital discharge, in addition to considerably increasing hospitalization costs, morbidity and mortality and the development of bronchopulmonary dysplasia (BPD) [4, 5]. Weaning is characterized as the process of withdrawing IMV and occupies approximately 40% of the time spent in ventilatory support. Both weaning and extubation must be performed early, but determining the exact moment to perform them is still a challenge in neonatal intensive care unit (NICU) [4-7].
Extubation is a process dependent on clinical judgment associated with the interpretation of ventilatory support, blood gas values, radiological examinations, and hemodynamic stability of the neonate [8]. It is defined as successful when there is no need for reintubation within a predefined period, which varies between institutions with observation windows from 12 h to 7 days post extubation [1, 9].
Extubation failure in PTNBs may occur due to a combination of factors, such as increased respiratory work, increased resistance due to upper airway narrowing, apneas and bradycardias associated with respiratory center immaturity. According to the literature, in the neonatal population, observation windows for failure vary from 2 to 7 days, and extubation failure rates can reach 40-50% [1, 3, 5, 8, 9].
Studies indicate a variability of weaning and extubation actions and practices, however, there is a scarcity of protocols in NICU. This is concerning, as the use of these protocols is intended to accelerate and manage the process of withdrawing the PTNB from the IMV [6, 10]. Other studies show that the existence of a protocol verifying the ability to initiate weaning reduces patients’ IMV time, and that a good weaning protocol must contain as fundamental components: actions that reduce ventilatory support, favoring patients’ acceptance of weaning; predetermined criteria that indicate suitability to start the spontaneous breathing test (SBT); standardized SBT; and the well-defined description of extubation failure criterion [4, 11]. Evidence shows that the use of SBT protocols developed and implemented in the NICU is becoming a strong predictor of success in extubation of PTNBs [10, 12]. In addition, studies mention the need for PTNBs to be adapted to noninvasive ventilatory support after extubation, addressing a reduction in the incidence of extubation failure in the period from 48 h to 7 days and highlighting the superiority of nasal intermittent positive pressure ventilation (NIPPV) when compared nasal continuous positive airway pressure (NCPAP) [13, 14].
Due to the existence of a variety of actions related to the weaning and extubation process and the scarcity of studies on the subject, it is important to know the ventilatory profile of PTNBs from the Centro Materno Infantil de Contagem (CMIC), in order to guarantee the improvement, quality and safety of care for these patients. In addition, due to the importance of the aforementioned children’s center in the State of Minas Gerais, as the reference for the Unified Health System (Sistema Unico de SaUde (SUS)) for the entire child population of Contagem, which is considered the third most populous municipality in the state of Minas Gerais, Brazil, it plays a crucial role. In addition, there are no specific extubation protocols for this population in this institution, making it necessary to elaborate them due to the exposed benefits. The protocol developed in this study can support future research on the subject, as well as support ventilatory assistance in PTNBs from other NICU.
Thus, this study aimed to present the ventilatory profile of premature infants submitted to IMV, assess the extubation failure rate and the elaboration of an extubation protocol.
| Materials and Methods | ▴Top |
Study type
This is a cross-sectional descriptive study, carried out in the NICU of the CMIC in the state of Minas Gerais, Brazil, carried out from August 2021 to January 2022.
Study population
PTNBs who were submitted to IMV for a period longer than 24 h and whose parents or legal guardians signed the Free and Informed Consent Term (FICT) participated in this study.
Sample
The sample was selected according to the flowchart shown in Figure 1. PTNBs with heart disease and/or congenital malformations, who were transferred to other institutions or died before the first extubation were excluded from the study. Heart diseases/congenital malformations were exclusion criteria from the sample because they could be confounding factors for the development of the extubation protocol, since each congenital malformation and/or heart disease has its peculiarities of evolution, with different clinical repercussions in relation to the extubation. Therefore, the developed protocol should be applicable to the majority of babies born in the maternity hospital in question, and in this case, it would be the population of premature newborns (NB). The final sample consisted of 27 PTNBs.
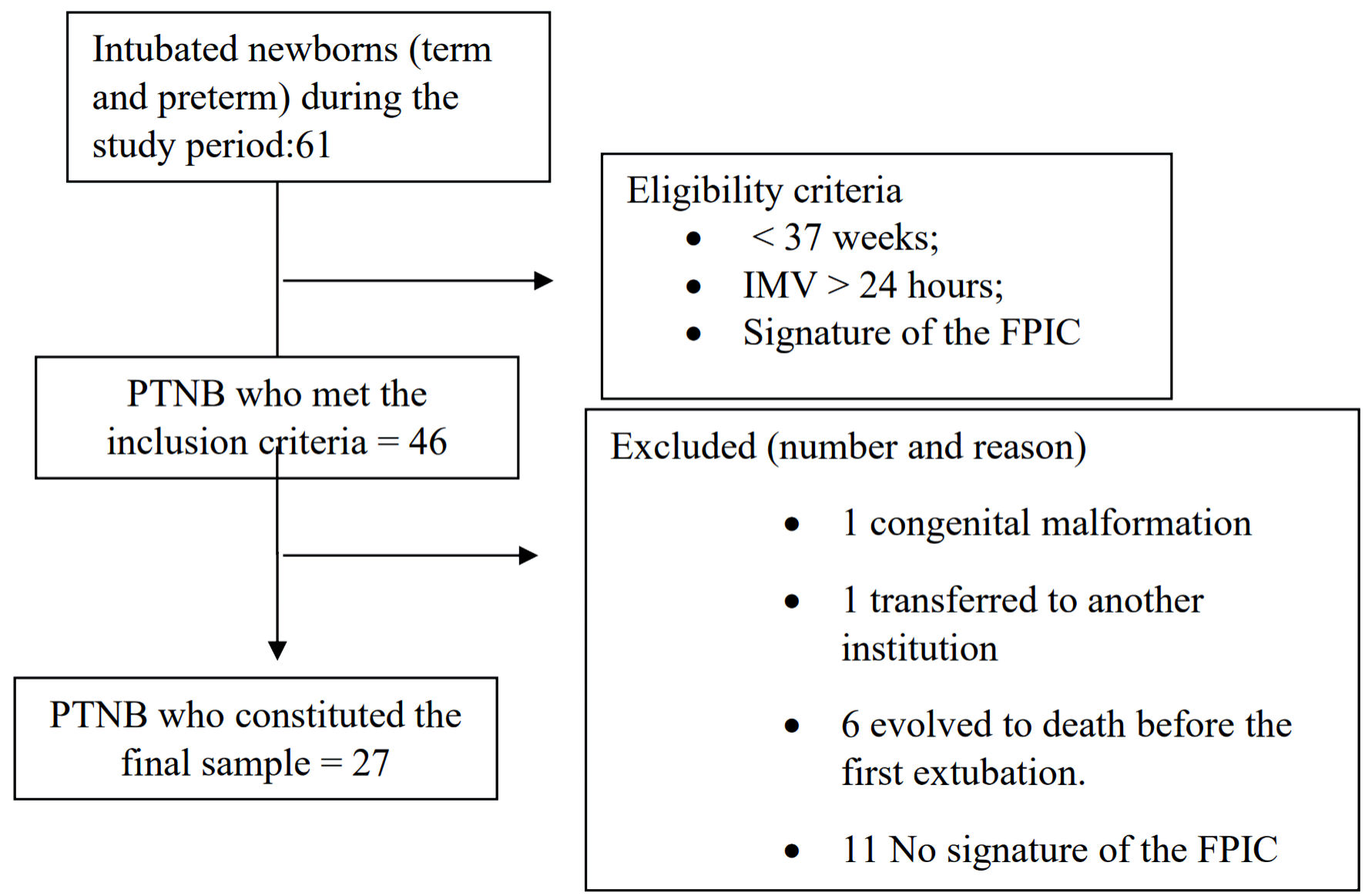 Click for large image | Figure 1. Sample selection process. Source: survey data. IMV: invasive mechanical ventilation; FPIC: free, prior and informed consent; PTNB: preterm newborn. |
Data collection
Data were collected through the records of the daily follow-up forms of the NICU physiotherapists and electronic medical records, encompassing all PTNBs who underwent endotracheal intubation. The collection was carried out by the author of the research, using the form developed for this purpose.
PTNBs were observed in the 7 days following extubation regarding the time between extubation and the need for reintubation and the main causes of failure. Extubation failure was considered to be those individuals who needed to be reintubated within 48 h after extubation.
Variables
The variables included in this study were: 1) Prenatal and birth period: use of antenatal corticosteroids, type of delivery, gestational age, birth weight, sex, Apgar (appearance, pulse, grimace, activity, and respiration) in the first and fifth minutes of life; 2) Pre-extubation moment: MV modality, ventilatory parameters, mean airway pressure (MAP), need for pre-extubation drug intervention, radiological and gasometric exams; 3) Post-extubation moment: type of post-extubation ventilatory support, presence of stridor, need for micronebulization and observation of the outcome of extubation.
The variables used were based on studies of Chawla et al [3], Shalish et al [8], Giaccone et al [9], Hartmann et al [11], Mandhari et al [12], Shalish et al [15], Ding et al [16], Shalish et al [17], Manley et al [18], Costa et al [19], Khemani et al [20], Kurtom et al [21], Cesar et al [22], Ambasta et al [23], and Gupta et al [24].
Preparation of the extubation protocol
For the construction of the extubation protocol, the results found in the research on the ventilatory profile of PTNBs, the post-extubation outcomes and the scientific evidence found in the National Library of Medicine (PubMed) in the MEDLINE databases and in the Latin American and Caribbean Literature on Health Sciences (Literatura Latino-Americana e do Caribe em Ciencias da Saude (LILACS)) database were considered.
Figures 2 and 3 show the elaborated protocol. The protocol was based on studies by Chawla et al [3], Shalish et al [8], Giaccone et al [9], Hartmann et al [11], Mandhari et al [12], and Gupta et al [24]. The studies addressed the main variables used in the assessment of pre-extubation PTNBs; however, they were used for the elaboration of the protocol.
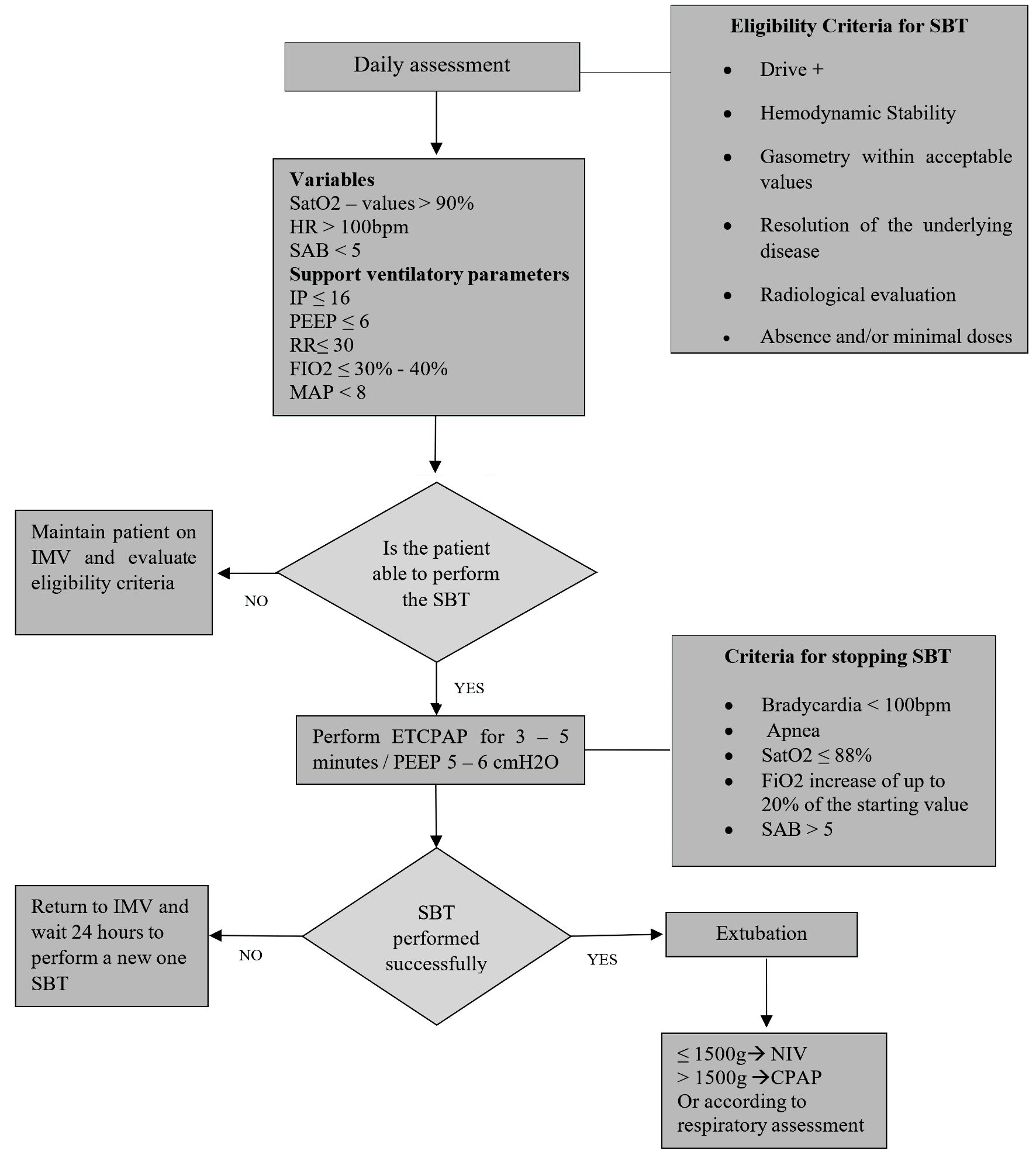 Click for large image | Figure 2. Protocol: weaning and extubation flowchart. SBT: spontaneous breathing test; HR: heart rate; SAB: Silverman-Andersen Bulletin; IP: inspiratory pressure; PEEP: positive end-expiratory pressure; RR: respiratory rate; FiO2: fraction of inspired oxygen; MAP: mean airway pressure; ETCPAP: endotracheal continuous positive airway pressure; IMV: invasive mechanical ventilation; NIV: noninvasive ventilation; CPAP: continuous positive airway pressure. |
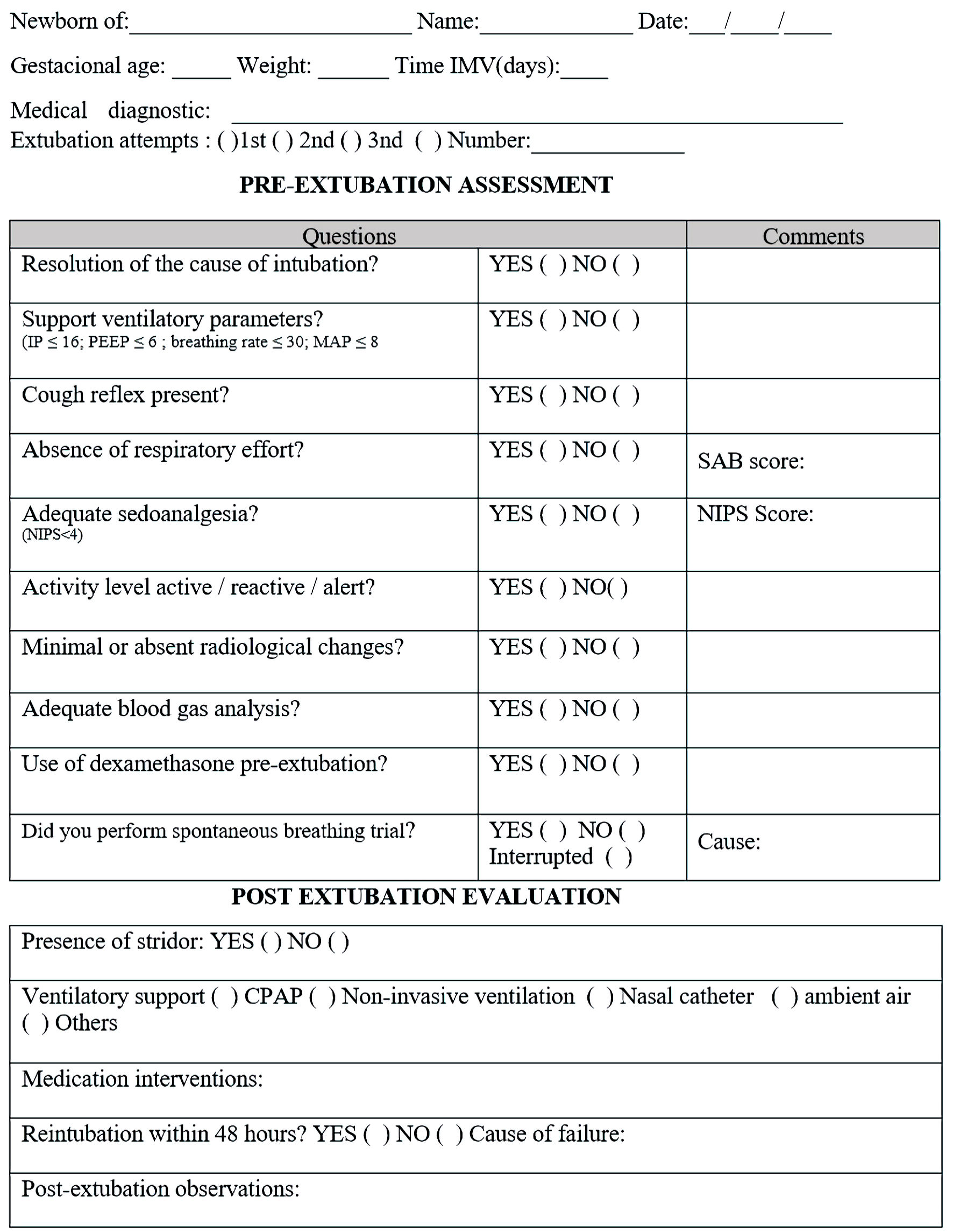 Click for large image | Figure 3. Extubation checklist. IMV: invasive mechanical ventilation; SAB: Silverman-Andersen Bulletin; NIPS: Neonatal Infant Pain Scale; CPAP: continuous positive airway pressure. |
The conduction flowchart (Fig. 2) and the extubation checklist (Fig. 3) developed in this study aimed to facilitate the assessment of the NB and be able to identify the opportune moment to carry out weaning and extubation. They are simple, practical and explanatory models in order to offer effective strategies to reduce MV time and, consequently, reduce the resulting risks, safely and early leading to the weaning and extubation process [3, 8, 9, 11, 12, 24].
Statistical analysis
Continuous descriptive data were presented as median, minimum, and maximum, according to data distribution. Categorical variables were presented in absolute values and percentages. The extubation failure rate was calculated as the number of extubation failure events divided by the total number of extubations performed, multiplied by 100, for the period from August 2021 to January 2022.
The total number of PTNBs was considered for sample characterization, and the total number of extubation events was analyzed to study the variables related to weaning from MV and extubation. To verify the normality of the data, the Shapiro Wilk test was used.
For statistical analysis, the Statistical Package for the Social Science (SPSS) software, version 25.0 was used.
Ethical aspects
The study was conducted in compliance with the ethical standards of the responsible institution regarding human subjects, following the current Brazilian ethical legislation (Resolution 466/2012, from the National Health Council). The study was approved by the Research Ethics Committee of Fundacao Hospitalar do Estado de Minas Gerais (CEPFHEMIG) under Ethical Opinion: 4,878,147, CAAE 48624321.7.0000.5119. All parents or legal guardians of the newborns provided written informed consent.
| Results | ▴Top |
A total of 27 PTNBs participated in this study, from which 43 extubation events originated. Table 1 presents the characteristics of premature NBs at the CMIC. It is observed that 55.6% (n = 15) of PTNBs are female, 59.3% (n = 16) were born by cesarean section, 51.9% (n = 14) were moderately premature and 74% (n = 20) weighed up to 1,499 g.
 Click to view | Table 1. Characteristics of Premature Newborns at Centro Materno Infantil de Contagem, Contagem/Minas Gerais (From August 2021 to January 2022) |
Table 2 shows the ventilatory and laboratory parameters at the pre-extubation moment. Regarding arterial blood gas analysis and pulmonary radiography, the absence or presence of these tests on the day of extubation was evaluated. It is noted that most NBs used the time-cycled, pressure-limited (TCPL) mechanical ventilation (MV) modality (97.7%). As for the ventilatory parameters, the median inspiratory pressure (IP) was 15, positive end-expiratory pressure (PEEP) was 6, respiratory rate (RR) was 30, and fraction of inspired oxygen (FiO2) was 30. Only 30.2% of PTNBs had MAP measured.
 Click to view | Table 2. Ventilatory and Laboratory Parameters Evaluated Before Extubation at the Centro Materno Infantil de Contagem, Contagem/Minas Gerais (From August 2021 to January 2022) |
Table 3 presents the outcome of extubation in relation to ventilatory support, medication and clinical variables. After extubation, there was a higher percentage of noninvasive ventilation (NIV) use among extreme (80%) and moderate (20%) preterm infants. Stridor was observed in 100% of the extreme and moderate preterm NBs in the event group with extubation failure, and micronebulization was not performed in any of these NBs. It was also observed that the drug intervention in this group was 20% (n = 1) in extremely preterm infants. Of the 43 extubation events analyzed, 84% (n = 36) were successful on the first attempt, 9% (n = 4) required up to three attempts, and 7% (n = 3) required more than three extubation attempts.
 Click to view | Table 3. Evaluation of the Extubation Outcome in Relation to Ventilatory Support, Medication and Clinical Variables of PTNBs from the Centro Materno Infantil de Contagem (From August 2021 to January 2022) |
Table 4 represents extubation failure rates according to age and birth weight. The overall extubation failure rate observed in the study, including all PTNBs, was 23.3%. When evaluating the failure rate according to gestational age, it is observed that the highest rate is found among PTNBs younger than 28 weeks (50%). Regarding failure rates according to birth weight ranges, extremely low weight PTNBs (less than 1,000 g) had the highest rates, followed by very low weight PTNBs (1,000 g to 1,499 g), with rates of 33, 3% and 21.4%, respectively. The main causes of extubation failure were apneas and severe respiratory failure, leading to reintubations within 48 h. It was observed in the 7 subsequent days through the evaluation of extubation events that seven PTNBs needed to return to invasive ventilatory support, totaling 19 reintubations.
 Click to view | Table 4. Extubation Failure Rates According to Age and Birth Weight at Centro Materno Infantil de Contagem - Contagem/Minas Gerais (From August 2021 to January 2022 (N = 43)) |
The conduction flowchart (Fig. 2) and the extubation checklist (Fig. 3) elaborated in this study facilitate the assessment of the NB and help to identify the opportune moment to carry out weaning and extubation. Simple, practical and explanatory models were developed in order to offer effective strategies to reduce MV time and, consequently, reduce the resulting risks, safely and early leading to the weaning and extubation process.
This is a pioneering study in the maternity unit under study, in which the ventilatory profile of PTNBs was analyzed in order to propose an extubation protocol. The main findings of this study were: 1) Moderate and extreme premature NBs and NBs weighing up to 1,499 g at birth were predominant in the sample. Prior to birth, 63% of PTNB mothers had received antenatal corticosteroid cycles. 2) At the time of extubation, PTNBs had minimum IMV parameters, but only 30% had their MAP assessed. In addition, 40% of them did not have arterial blood gases and 49% did not have radiography before extubation. 3) The overall extubation failure rate of PTNBs was 23% from August 2021 to January 2022. When we stratify this rate according to gestational age and birth weight, the highest rates are found in smaller NBs (28 weeks (50%) and less than 1,449 g (33%)). 4) The main causes of extubation failure in PTNBs were apnea and severe respiratory failure caused by severe respiratory effort associated with bradycardias and desaturation. Additionally, stridor presented in 100% of extreme and moderate PTNBs in the event with failure of extubation group.
| Discussion | ▴Top |
In the present study, the ventilatory profile of PTNBs was analyzed, and it was evidenced that the variables gestational age less than 32 weeks and birth weight less than 1,500 g were predominant among the participants. It is known that these variables are factors that may contribute to the need for NBs to return to IMV, being exposed to greater risks of morbidity and mortality, characterizing as a risk factor with a percentage of up to 70%. Furthermore, when PTNBs are submitted to reintubations and prolonged use of IMV, they predispose to the development of BPD and consequently prolonged hospital stay [1, 5, 10, 15-19]. This fact corroborates the findings of this study, where 50% of PTNBs who failed extubation had a GA < 28 weeks, and 74% weighed less than 1,500 g, but this rate is related to extubation events, which directly influences a high failure rate, since most events occurred with extremely preterm infants.
The overall extubation failure rate observed in the study was 23.3%, a relatively lower value compared to that reported in the literature, which varies between 40% and 50% [1, 3]. However, it should be considered that the analysis performed in this study had a short period with a minimum sample of 27 PTNBs, in addition to the fact that the failure rate evidenced is related to the extubation events performed and not to the sample of the study. Although the failure rate of the present study was calculated considering reintubations within 48 h after extubation, it was observed through the evaluation of extubation events that seven PTNBs needed to return to invasive ventilatory support within a period of up to 7 days post extubation, totaling 19 reintubations.
The blood gas alterations may have an unfavorable outcome in extubation [19]. In this study, it was identified that 39.5% of PTNBs did not undergo pre-extubation blood gas analysis. Laboratory and chest radiology tests, together with the interpretation of ventilatory support and hemodynamic stability of the PTNB, will determine the possibility of performing the extubation process [8, 18]. Changes not identified before extubation may contribute to its failure, since increased or low pH and bicarbonate values are associated with risks of extubation failure [19]. The extubation criteria are still not well clarified in the literature, so it is important to standardize them and evaluate accurate predictors for the procedure, since the exact moment for extubation is still a challenge in NICU [7], which emphasizes the need for strategies that increase the chance of successful extubation.
According to the results presented in this study, the presence of stridor in extremely and moderately preterm infants was predominant, especially in the group that had extubation failure. However, post-extubation micronebulization was not performed in any of them and, in addition, only 13 (30.2%) of these PTNBs received pre-extubation drug intervention, with a percentage of 69.8% for not performing any type of pre-extubation intervention. This fact may have directly influenced these failures, and studies have already demonstrated success in extubation in PTNBs who received dexamethasone days or hours before the procedure, reporting a reduction in the number of reintubations, as well as the performance of micronebulization with adrenaline for those who had stridor [20, 21]. NBs have specific anatomical characteristics of the airways, which make them more susceptible to risk of injury during the intubation process, and consequently predisposition to present stridor due to post-extubation glottic edema [22].
The presence of stridor evidenced in this study is related to greater chances of reintubation, since PTNBs who had successful extubation had minimal rates of stridor compared to those who failed. In addition, it was observed that in the group with successful extubation events, 78.1% of extreme and moderate preterm infants received pre-extubation drug intervention, and 14.3% of these received post-extubation micronebulization. In addition to stridor, apnea and severe respiratory effort were also one of the main causes of reintubation in PTNBs. Severe respiratory effort can be identified through the Silverman-Andersen Bulletin (BSA), an objective and quick-to-execute tool, which aims to grade the respiratory effort presented by the PTNB, thus being able to identify the opportune moment for the change in the level of ventilatory support [25]. Considering the results found in the present study and in the literature, we can highlight the benefits and importance of pre- and post-extubation interventions [20, 22-24]. In addition, pain assessment in these PTNBs is opportune, since they are often submitted to invasive procedures, such as endotracheal and nasopharyngeal aspirations, which are painful processes that directly influence stability, clinical evolution and neonatal morbidity [26, 27]. The Neonatal Infant Pain Scale (NIPS) is a validated instrument capable of reliably assessing PTNB pain and, through the information provided, it will be possible to determine the appropriate interventions for pain relief [28].
The use of NIV has been recommended as an option for post-extubation ventilatory support in PTNBs, being offered through NCPAP or NIPPV [14]. Initially, nasal CPAP was the most used support after extubation in preterm infants, but when compared with NIPPV, a reduction in extubation failure rates was observed, along with significant improvement in neonatal outcomes [16, 24, 29]. In the present study, the predominant use of NIV was observed, both in the group of successful and failed extubation events. It is important to effectively assess the respiratory conditions of PTNBs after extubation, to determine the most appropriate support to be used.
Knowing the ventilatory profile of preterm infants and the risk factors associated with extubation failure facilitates the weaning process and increases the chance of successful extubation. In a study carried out in Toronto, an evidence-based SBT protocol was developed with the aim of improving extubation rates and promoting the minimization of MV. The study was carried out in two periods of time, before and after the implementation of the protocol, where the result was effective in reducing the extubation failure rate from 9.9% to 4.1% [12].
This study had limitations inherent to cross-sectional studies, such as the impossibility of attesting a causal relationship; the study was performed at a single center so generalization of findings should be done with caution. However, it is noteworthy that this is the first study that identified the ventilatory profile of PTNBs in this maternity hospital, being an important starting point for conducting future research. In addition, the advantage of this study was the development of an extubation protocol for the NICU of the maternity unit under study, which can bring benefits to this population, systematizing the assessment of the pre-extubation moment and the surveillance of the post-extubation moment, thus being able to reduce failure rates and consequently the sequelae caused by prolonged hospitalization.
Conclusions
It is concluded that gestational age and birth weight were variables associated with a higher rate of extubation failure, due to the lack of preventive actions before and after extubation. Therefore, it is important to emphasize the need for defined strategies and actions that promote early yet safe weaning and extubation. While the weaning protocol presented is scientifically grounded, its implementation in the NICU and subsequent evaluation of its impact on PTNBs are essential.
Acknowledgments
We thank all those who contributed directly and indirectly to the development of this research, including the parents and legal guardians of the children involved.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Jhennif Sabrina da Silva: conception, data collection, data analysis, and manuscript writing. Valeria Emiliane Lopes Moura: data collection and manuscript review. Ana Cristina de Oliveira Costa: initial translation and manuscript review. Ana Carolina Gomide Micheletti Gomide Nogueira de Sa: study design and manuscript review. Isabella Diniz Faria: study design, data analysis, manuscript review, and final review.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
PTNBs: preterm newborns; NICU: neonatal intensive care unit; IMV: invasive mechanical ventilation; BPD: bronchopulmonary dysplasia; SBT: spontaneous breathing test; NIPPV: nasal intermittent positive pressure ventilation; NCPAP: nasal continuous positive airway pressure; SUS: Sistema Unico de Saude; CMIC: Centro Materno Infantil de Contagem; FICT: Free and Informed Consent Term; MAP: mean airway pressure; CEPFHEMIG: Research Ethics Committee of Fundacao Hospitalar do Estado de Minas Gerais
| References | ▴Top |
- Jurkevicz R, Andreazza MG, Gomes EO, Oliveira ALS, Gallo RBS. Sucesso e falha de extubacao em recem-nascidos prematuros ate 32 semanas de idade gestacional TT - Success and failure of extubation in premature newborns up to 32 weeks of gestational age. Rev Pesqui Fisioter. 2021;11(1):155-162.
doi - Andrade LB, Melo TM, Morais DF, Lima MR, Albuquerque EC, Martimiano PH. Spontaneous breathing trial evaluation in preterm newborns extubation. Rev Bras Ter Intensiva. 2010;22(2):159-165.
pubmed - Chawla S, Natarajan G, Shankaran S, Carper B, Brion LP, Keszler M, Carlo WA, et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J Pediatr. 2017;189:113-119.e112.
doi pubmed pmc - Lourencao ML, Carvalho WB. Pediatric ventilation weaning. Rev Bras Ter Intensiva. 2020;32(3):333-336.
doi pubmed pmc - Hermeto F, Martins BM, Ramos JR, Bhering CA, Sant'Anna GM. Incidence and main risk factors associated with extubation failure in newborns with birth weight < 1,250 grams. J Pediatr (Rio J). 2009;85(5):397-402.
doi pubmed - Bacci S, Pereira JM, Chagas A, Carvalho LR, Azevedo V. Role of physical therapists in the weaning and extubation procedures of pediatric and neonatal intensive care units: a survey. Braz J Phys Ther. 2019;23(4):317-323.
doi pubmed pmc - Bacci S, Johnston C, Hattori WT, Pereira JM, Azevedo V. Mechanical ventilation weaning practices in neonatal and pediatric ICUs in Brazil: the Weaning Survey-Brazil. J Bras Pneumol. 2020;46(4):e20190005.
doi pubmed pmc - Shalish W, Kanbar L, Kovacs L, Chawla S, Keszler M, Rao S, Latremouille S, et al. Assessment of extubation readiness using spontaneous breathing trials in extremely preterm neonates. JAMA Pediatr. 2020;174(2):178-185.
doi pubmed pmc - Giaccone A, Jensen E, Davis P, Schmidt B. Definitions of extubation success in very premature infants: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2014;99(2):F124-127.
doi pubmed pmc - Shalish W, Kanbar LJ, Rao S, Robles-Rubio CA, Kovacs L, Chawla S, Keszler M, et al. Prediction of Extubation readiness in extremely preterm infants by the automated analysis of cardiorespiratory behavior: study protocol. BMC Pediatr. 2017;17(1):167.
doi pubmed pmc - Hartmann SM, Zimmerman JJ. Standardization of ventilator weaning benefits both researchers and clinicians. Crit Care Med. 2017;45(1):139-140.
doi pubmed - Mandhari H Al, Finelli M, Chen S, Tomlinson C, Nonoyama ML. Effects of an extubation readiness test protocol at a tertiary care fully outborn neonatal intensive care unit. Can J Respir Ther. 2019;55(1):81-88.
doi - Ferguson KN, Roberts CT, Manley BJ, Davis PG. Interventions to improve rates of successful extubation in preterm infants: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(2):165-174.
doi pubmed - Lemyre B, Davis PG, De Paoli AG, Kirpalani H. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev. 2017;2(2):CD003212.
doi pubmed pmc - Shalish W, Keszler M, Davis PG, Sant'Anna GM. Decision to extubate extremely preterm infants: art, science or gamble? Arch Dis Child Fetal Neonatal Ed. 2022;107(1):105-112.
doi pubmed - Ding F, Zhang J, Zhang W, Zhao Q, Cheng Z, Wang Y, Bo T, et al. Clinical study of different modes of non-invasive ventilation treatment in preterm infants with respiratory distress syndrome after extubation. Front Pediatr. 2020;8:63.
doi pubmed pmc - Shalish W, Latremouille S, Papenburg J, Sant'Anna GM. Predictors of extubation readiness in preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2019;104(1):F89-F97.
doi pubmed - Manley BJ, Doyle LW, Owen LS, Davis PG. Extubating extremely preterm infants: predictors of success and outcomes following failure. J Pediatr. 2016;173:45-49.
doi pubmed - Costa AC, Schettino Rde C, Ferreira SC. [Predictors of extubation failure and reintubation in newborn infants subjected to mechanical ventilation]. Rev Bras Ter Intensiva. 2014;26(1):51-56.
doi pubmed pmc - Khemani RG, Randolph A, Markovitz B. Corticosteroids for the prevention and treatment of post-extubation stridor in neonates, children and adults. Cochrane Database Syst Rev. 2009;2009(3):CD001000.
doi pubmed pmc - Kurtom W, Schmidt A, Jain D, Vanbuskirk S, Schott A, Bancalari E, Claure N. Efficacy of late postnatal dexamethasone on weaning from invasive mechanical ventilation in extreme premature infants. J Perinatol. 2021;41(8):1951-1955.
doi pubmed pmc - Cesar RG, de Carvalho WB. L-epinephrine and dexamethasone in postextubation airway obstruction: a prospective, randomized, double-blind placebo-controlled study. Int J Pediatr Otorhinolaryngol. 2009;73(12):1639-1643.
doi pubmed - Ambasta S, Rudingwa P, Kundra P, Gnanasekar R. Treatment of upper airway oedema prior to extubation. Indian J Anaesth. 2016;60(10):777-778.
doi pubmed pmc - Gupta D, Greenberg RG, Sharma A, Natarajan G, Cotten M, Thomas R, Chawla S. A predictive model for extubation readiness in extremely preterm infants. J Perinatol. 2019;39(12):1663-1669.
doi pubmed - Hedstrom AB, Gove NE, Mayock DE, Batra M. Performance of the silverman andersen respiratory severity score in predicting PCO(2) and respiratory support in newborns: a prospective cohort study. J Perinatol. 2018;38(5):505-511.
doi pubmed pmc - Nicolau CM, Pigo JDC, Bueno M, Falcao MC. Avaliacao da dor em recem-nascidos prematuros durante a fisioterapia respiratoria. Rev Bras Saude Matern Infant. 2008;8(3):285-290.
doi - Andreazza MG, Motter AA, Cat ML, da Silva RPGVC. Pain relief in premature neonates during upper airway aspiration comparing positions. Rev Pesqui em Fisioter. 2020;10(4):674-682.
doi - Motta Gde C, Schardosim JM, Cunha ML. Neonatal infant pain scale: cross-cultural adaptation and validation in Brazil. J Pain Symptom Manage. 2015;50(3):394-401.
doi pubmed - Nasef N, Rashed HM, Aly H. Practical aspects on the use of non-invasive respiratory support in preterm infants. Int J Pediatr Adolesc Med. 2020;7(1):19-25.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
