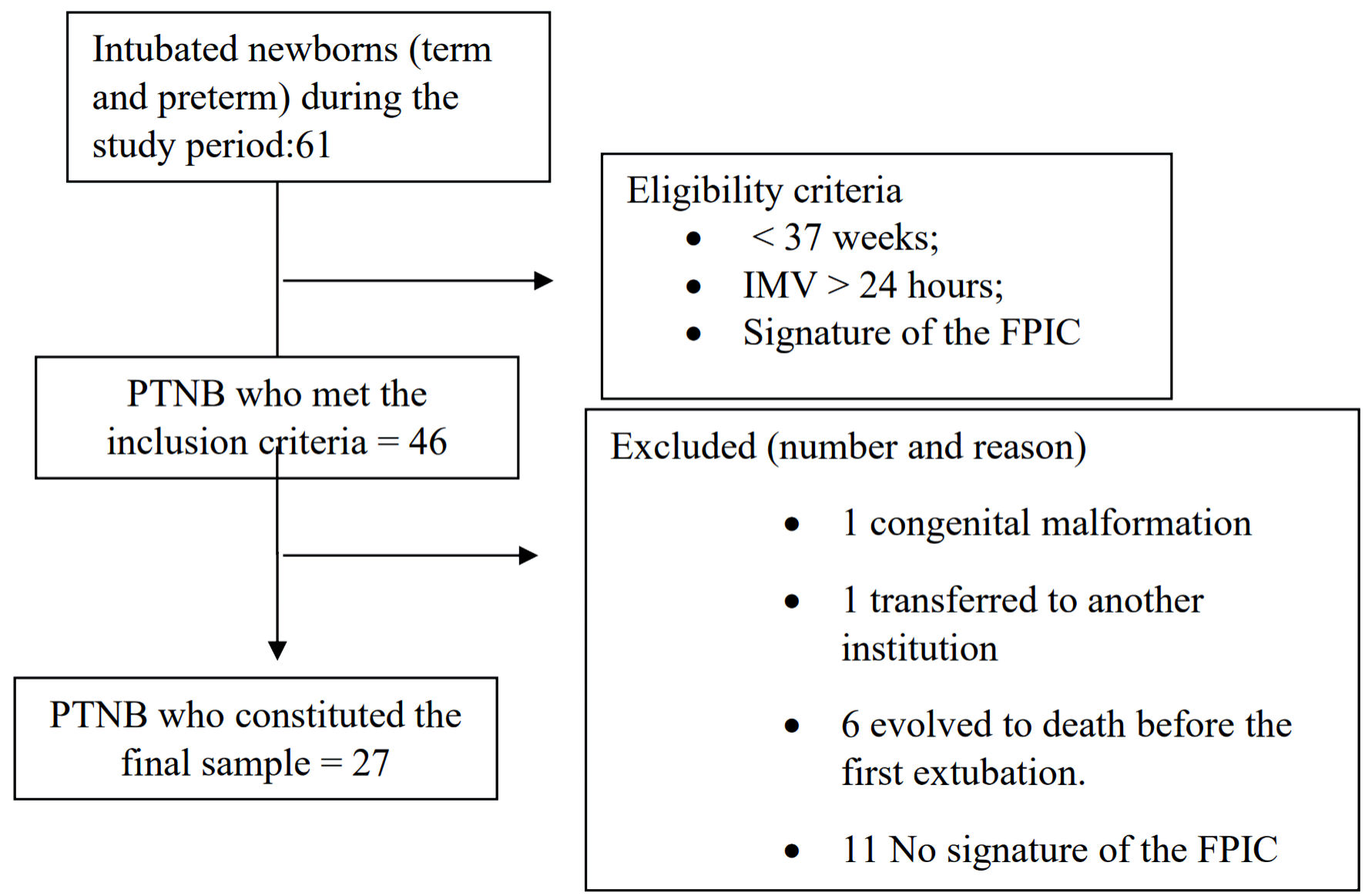
Figure 1. Sample selection process. Source: survey data. IMV: invasive mechanical ventilation; FPIC: free, prior and informed consent; PTNB: preterm newborn.
| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website https://www.theijcp.org |
Original Article
Volume 13, Number 3, December 2024, pages 86-95
Weaning From Mechanical Ventilation in Preterm Newborns: Ventilatory Profile and the Construction of an Extubation Protocol
Figures
Tables
| Variable | N = 27 |
|---|---|
| Data were presented in absolute frequency and percentage, n represents the sample and % the relative frequency (%) or amedian, minimum and maximum. Apgar: appearance, pulse, grimace, activity, and respiration. | |
| Gender (n, %) | |
| Male | 12 (44,4%) |
| Female | 15 (55,6%) |
| Type of delivery (n, %) | |
| Natural/vaginal | 11 (40,7%) |
| Cesarean section | 16 (59,3%) |
| Antenatal corticosteroid (n, %) | |
| Yes | 17 (63,0%) |
| No | 10 (37,0%) |
| Gestational age (n, %) | |
| Extremely premature (< 28 weeks) | 7 (25,9%) |
| Moderately premature (28 to 31 weeks and 6 days) | 14 (51,9%) |
| Late premature (32 to 36 weeks + 6 days) | 6 (22,2%) |
| Weight at birth (n, %) | |
| Extremely low weight (less than 1,000 g) | 10 (37,0%) |
| Very low weight (1,000 to 1,499 g) | 10 (37,0%) |
| Low weight (1,500 to 2,499 g) | 5 (18,5%) |
| Over 2,500 g | 2 (7,4%) |
| Apgar score (median, minimum and maximuma) | |
| Apgar - 1st min | 8 (0 - 9) |
| Apgar - 5th min | 9 (0 - 10) |
| Variable | N = 43 |
|---|---|
| Data were presented in frequency and percentage (n, %) or amedian, minimum and maximum. TCPL: pressure-limited time-cycled ventilation; PCV: pressure-controlled ventilation; IP: inspiratory pressure; PEEP: positive end-expiratory pressure; RR: respiratory rate; FiO2: fraction of inspired oxygen; MAP: mean airway pressure. | |
| Type of mechanical ventilation, n (%) | |
| TCPL | 42 (97.7%) |
| PCV | 1 (2.3%) |
| Ventilatory parameters (median, minimum - maximum)a | |
| IP | 15 (12 - 17) |
| PEEP | 6 (5 - 7) |
| RR | 30 (24 - 36) |
| FiO2 | 30 (21 - 50) |
| MAP evaluation, n (%) | |
| Yes | 13 (30.2%) |
| No | 30 (69.8%) |
| Arterial blood gases, n (%) | |
| Yes | 26 (60.5%) |
| No | 17 (39.5%) |
| Pulmonary X-ray, n (%) | |
| Yes | 22 (51.2%) |
| No | 21 (48.8%) |
| Drug intervention, n (%) | |
| Yes | 13 (30.2%) |
| No | 30 (69.8%) |
| Assessment of extubation events (n = 43) | ||||||
|---|---|---|---|---|---|---|
| Events with successful extubation (n = 33) | Events with failed extubation (n = 10) | |||||
| Extreme (n = 5) | Moderate (n = 21) | Late (n = 7) | Extremes (n = 5) | Moderate (n = 2) | Later (n = 3) | |
| Data were presented in frequency and percentage. NIV: noninvasive ventilation; CPAP: continuous positive airway pressure; Apgar: appearance, pulse, grimace, activity, and respiration. | ||||||
| Ventilatory support, n (%) | ||||||
| NIV | 4 (80.0) | 16 (72.2) | 0 (0.0) | 5 (100.0) | 2 (100.0) | 3 (100.0) |
| CPAP | 1 (20.0) | 5 (23.8) | 4 (57.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Ambient air | 0 (0.0) | 0 (0.0) | 3 (42.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Presence of stridor, n (%) | 0 (0.0) | 2 (9.5) | 1 (14.3) | 5 (100.0) | 2 (100.0) | 2 (66.7) |
| Post-extubation micronebulization | 0 (0.0) | 3 (14.3) | 1 (14.3) | 0 (0.0) | 0 (0.0) | 2 (66.7) |
| Drug intervention | 2 (40.0) | 8 (38.1) | 0 (0.0) | 1 (20.0) | 0 (0.0) | 2 (66.7) |
| Pre-extubation 5th min Apgar up to 3 points at birth | 0 (0.0) | 0 (0.0) | 1 (14.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Variable | Failure rate (%) |
|---|---|
| Extubation failure rate (reintubations within 48 h): total number of extubation failures divided by the total number of extubations × 100 (From August to January 2022). | |
| General fee | 23.3% |
| Gestational age | |
| Extremely premature (< 28 weeks) | 50% |
| Moderately premature (28 to 31 weeks and 6 days) | 8.7% |
| Late premature (32 to 36 weeks + 6 days) | 30% |
| Birth weight | |
| Extremely low weight (less than 1,000 g) | 33.3% |
| Very low weight (1,000 to 1,499 g) | 21.4% |
| Low weight (1,500 to 2,499 g) | 0% |
| Over 2,500 g | 0% |