| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website http://www.theijcp.org |
Case Report
Volume 4, Number 2-3, October 2015, pages 162-165
Retroperitoneal Arteriovenous Malformation: A Rare Cause of Pulmonary Hypertension in a Premature Infant
Maksim Zaguraa, d, Heleri Konika, Helgi Padarib, Tuuli Metsvahtb, Toomas Hermlina, Liis Salumaec, Tiiu Tomberga
aRadiology Clinic, Tartu University Hospital, Tartu, Estonia
bAnaesthesiology and Intensive Care Clinic, Tartu University Hospital, Tartu, Estonia
cDepartment of Clinical Pathology/Cytology, Karolinska University Hospital, Stockholm, Sweden
dCorresponding Author: Maksim Zagura, Radiology Clinic, Tartu University Hospital, 8 Puusepa Street, Tartu 51014, Estonia
Manuscript accepted for publication August 18, 2015
Short title: Retroperitoneal Arteriovenous Malformation
doi: http://dx.doi.org/10.14740/ijcp214w
| Abstract | ▴Top |
Retroperitoneal arteriovenous malformations (AVMs) are rare lesions consisting of dysplastic vessels, which may produce diverse clinical features. We report a case of premature neonate born on the 29th week of gestation, who presented with heart failure, generalized edema, respiratory dyspnea and metabolic acidosis. Digital subtraction angiography revealed a large AVM located adjacent to the aorta and the inferior vena cava. Lumbar arteries supplying the AVM were occluded by coils. The AVM was partially embolized using N-butyl cyanoacrylate. Despite apparently successful embolization procedure, heart failure and respiratory distress progressed. The newborn died on her fourth day of life. We report the first case describing AVM embolization in a very low birth weight preterm infant.
Keywords: Arteriovenous malformation; Preterm infant; Pulmonary hypertension; Hydrops; Embolization; Ultrasound
| Introduction | ▴Top |
High flow vascular malformations may lead to congestive heart failure. The currently available classification of the International Society for the Study of Vascular Anomalies (ISSVA) defines arteriovenous malformation (AVM) as nidus containing fast flow network of dysplastic arteries and veins [1]. The most frequent location of AVMs in neonates is liver, whereas lung and brain AVMs are silghtly less common [2]. Diagnosis can be complicated at birth as the clinical features of AVMs are variable and may occur with a long latency period. Previous research regarding endovascular treatment of AVMs in preterm infants is limited. We report for the first time a unique case of a large retroperitoneal AVM, which was treated with transarterial embolization in a very low weight preterm infant.
| Case Report | ▴Top |
A primipara 23-year-old woman presented with the complaint of abdominal tension and decreased fetal movements during couple last days. Hydrops and fetal distress with umbilical arterial blood flow of II-III class was diagnosed. A girl was born by emergency caesarean section in general anesthesia at gestational age of 28 weeks and 1 day with birth weight of 1,355 g. Apgar scores were 4, 5 and 6 at 1, 5 and 10 min, respectively. The baby was intubated and surfactant was given immediately after birth due to severe respiratory failure. Blood analysis revealed anemia, thrombocytopenia, hypoproteinemia and elevated level of lactate. Arterial blood gas analysis showed pH 7.29, base excess (BE) -5 mmol/L and pCO2 44 mm Hg. Dobutamine, adrenaline infusions and albumin bolus for hemodynamic stabilization were given. Anemia and thrombocytopenia were corrected.
Echocardiography (ECHO) showed right-heart enlargement with suprasystemic right ventricular pressure up to 68 mm Hg and right-to-left shunt through persistent ductus arteriosus. Left ventricular function was normal: fractional shortening (FS) of 29% and ejection fraction (EF) of 60% were measured. In abdominal ultrasound (US), suprarenal part of the inferior vena cava (IVC) was significantly dilated measuring 25 × 38 mm. Moreover, an inhomogenic vascular mass adjacent to the aorta and IVC was revealed. The lesion contained focal color voids on Doppler ultrasound, suggesting thrombosis. In renal arteries, monophasic flow with dampened peak systolic velocity was demonstrated. Based on these findings, a steal syndrome was suspected.
The condition of the newborn remained unstable, and severe metabolic acidosis and lactacidemia persisted. At the age of 18 h intravenous digital subtraction angiography (iDSA) was performed. Vascular lesion with size up to 3 cm was diagnosed. Blood supply from lumbar arteries and steal syndrome from visceral arteries were recorded. The AVM drained into the IVC through a 6 mm wide vascular channel (Fig. 1A, B). Coil embolization of fourth and fifth lumbar arteries was performed successfully. The upper part of AVM was embolized by injection of N-butyl cyanoacrylate glue. After the embolization, the blood flow through the AVM was significantly reduced. Repeated ECHO showed a decrease in right atrial and ventricular dilatation. However, left ventricular systolic function deteriorated: FS 24%, EF 52%.
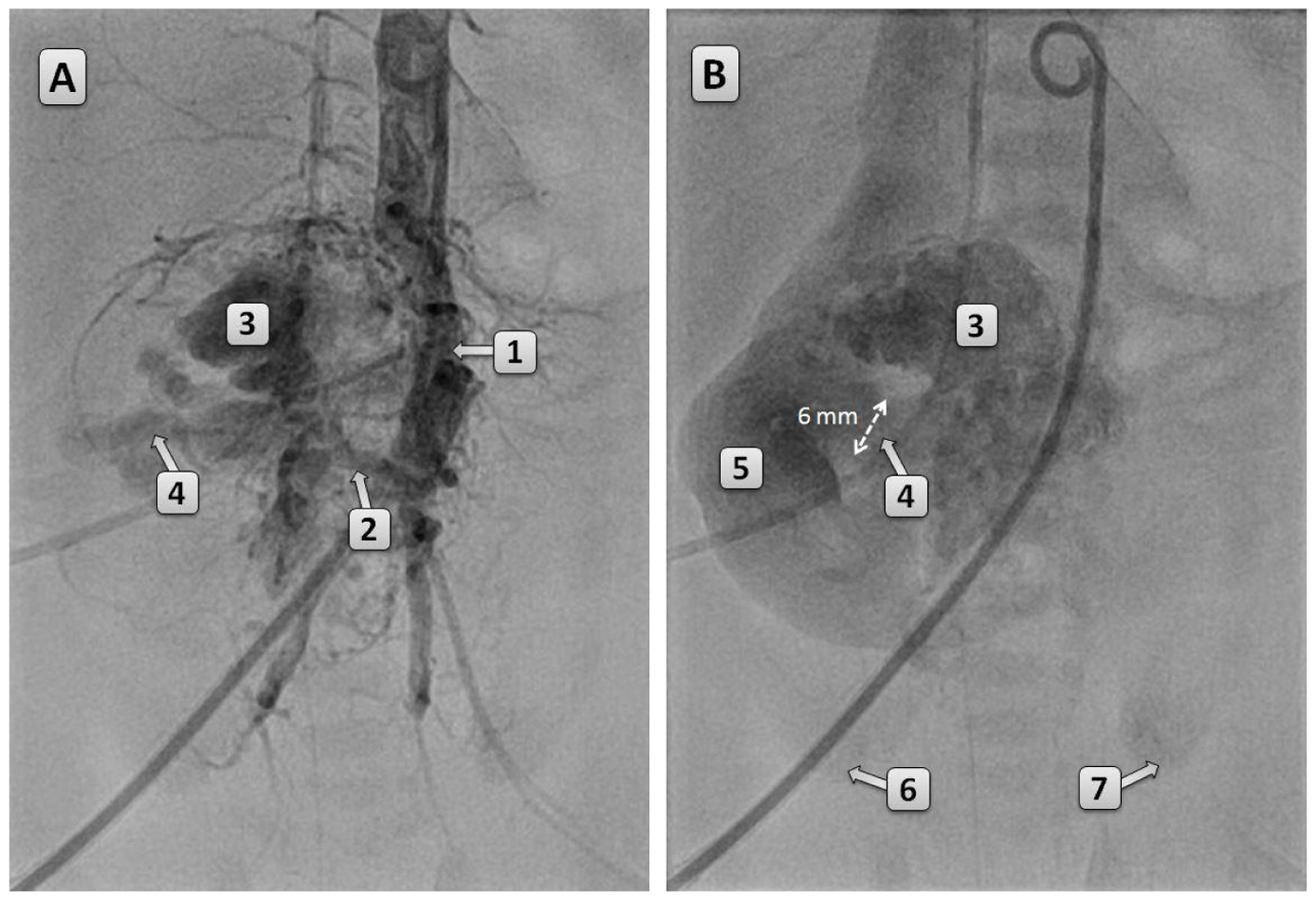 Click for large image | Figure 1. (A, B) DSA of the aorta performed at the age of 18 h. The aorta is dislocated to the left by the AVM. Blood supply of the AVM occurs through the lumbar arteries. In (B), a 6 mm shunt between the AVM and IVC can be seen. Renal perfusion is decreased as there is only slight enhancement at the lower poles of the kidneys. 1: abdominal aorta; 2: feeding vessel of the AVM; 3: AVM; 4: shunt between AVM and the IVC; 5: IVC; 6: lower pole of the right kidney; 7: lower pole of the left kidney. |
During iDSA, the baby was hemodynamically unstable: severe acidosis with pH 6.9, BE < -20 mmol/L and lactate > 20 mmol/L were observed. At the end of the procedure, high frequency oscillatory ventilation was started, several tris-hydroxymethyl aminomethane (THAM) boluses were administered and continuous furosemide infusion was added. With the treatment acid-base balance improved, pH 7.25 and BE -14 were recorded, but lactate level remained > 20 mmol/L and severe hypoxia persisted. The baby died at the age of 85 h.
At autopsy, a cystic lesion measuring 4 × 3.5 × 3.5 cm was found (Fig. 2A, B). A thrombus was revealed on the right side of the lesion. Most part of the prerenal IVC was in close contact with the AVM. On histological analysis, the AVM consisted of dilated vascular spaces filled with blood. Based on histological and immunohistochemical studies, an AVM with primitive cellular components was diagnosed.
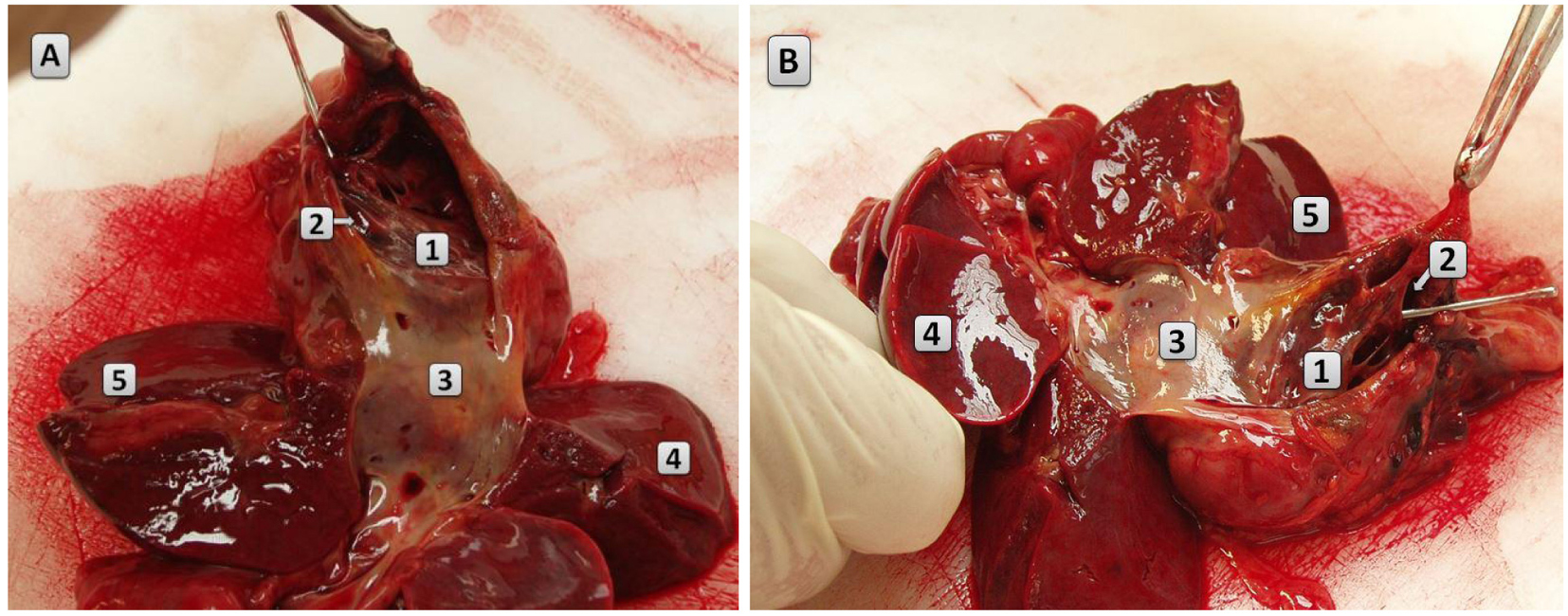 Click for large image | Figure 2. (A, B) Macroscopic picture of the AVM. The IVC and the liver are dissected. The AVM is composed of cystic cavities and it encircles most of the suprarenal part of the IVC. 1: AVM; 2: metal probe is inserted in the shunt connecting the AVM and the aorta; 3: IVC; 4: right lobe of the liver; 5: left lobe of the liver. |
| Discussion | ▴Top |
According to our knowledge, there are no previous case reports regarding embolization of true AVMs in very low birth weight neonates. Thukaram and co-authors reported a case of a 1,400 g premature infant, who underwent coil embolization of patent ductus arteriosus [3]. In another report, endovascular embolization of vein of Galen aneurysm was performed in a preterm infant [4]. In our patient, the fourth and fifth lumbar arteries feeding the AVM were embolized with coils. Furthermore, embolization of the AVM with N-butyl cyanoacrylate glue was carried out, following which a decrease in flow through the AVM was observed. Follow-up ECHO showed reduction in right atrial dilatation. However, due to prolonged hypoperfusion and irreversible damage of vital organs, the clinical condition of the infant rapidly deteriorated and she died on the fourth day of life.
Retroperitoneal AVMs should be differentiated from a variety of underlying conditions causing congestive heart failure. Sonography, magnetic resonance imaging (MRI) and DSA represent the cornerstone for morphological characterization of AVMs and facilitate their differentiation from other vascular anomalies [5]. A case of arteriovenous fistula arising from the descending aorta and draining into superior vena cava and the azygos vein was described in a 14-month-old girl [6]. In another case report, a retroperitoneal undifferentiated sarcoma adjacent to the aortic bifurcation, iliac vessels and IVC was diagnosed by DSA in a 3-month-old infant [7]. As liver is the most common location of AVMs in neonates, there are numerous reports on congestive heart failure in patients with hepatic AVMs [8]. However, as there is a broad spectrum of high-flow vascular lesions, the term “AVM” has been used inconsistently in the literature [7]. It is important to differentiate AVMs from hemangiomas, which are the most common vascular tumors. Hemangiomas are surrounded by abundant fibrous tissue, whereas AVMs are usually associated with the limited amount of soft tissue mass. In our patient, a vascular lesion connected to the IVC and several lumbar arteries was shown both on the abdominal ultrasound and the iDSA. As the lesion contained soft tissue components, a vascular tumor was suspected. However, histological analysis revealed the presence of cellular-rich primitive areas adjacent to dysplastic vascular channels. Thus, in some cases AVMs and hemangiomas cannot be differentiated based solely on the findings of radiologic imaging studies and histological examination is necessary. Moreover, AVMs should be differentiated from arteriovenous fistulas, which are characterized by a single communication between an artery and a vein. In contrast, AVMs have multiple communications between arterial and venous system [5]. In our case, a true AVM containing large nidus of dysplastic vessels was revealed. Our case is unique because the AVMs involving major retroperitoneal blood vessels in preterm infants occur very rarely.
Pulmonary hypertension leads to shunting of non-oxygenated blood from the pulmonary to the systemic circulation and it is an important determinant of mortality in neonates [9]. The main cause of pulmonary hypertension in AVMs is increase in pulmonary blood flow [8]. In our patient, ECHO demonstrated enlarged right ventricle and increase in right ventricular pressure. Furthermore, right-to-left shunt through the ductus arteriosus was demonstrated. Similarly to previous reports [8], our findings underline the importance of early diagnosis of pulmonary hypertension and its underlying mechanism, which affects the treatment strategy. We would like to emphasize that inhaled nitric oxide should be used with caution in patients with pulmonary hypertension caused by AVMs, who present with increased pulmonary blood flow. Due to its vasodilatory effects, nitric oxide would further increase pulmonary perfusion and could exacerbate pulmonary hypertension [8]. In patients with pulmonary hypertension caused by an AVM, treatment should be aimed at occlusion of arteriovenous shunts to decrease pulmonary blood flow.
Heart failure is a common complication of AVMs with large arteriovenous shunts. In neonates with heart failure, ECHO is usually the imaging modality of the first choice. However, if congenital heart defects are excluded, US scans of brain and abdomen would be necessary to diagnose possible vascular anomalies. Major advantages of US include wide availability, suitability for bedside use and lack of radiation exposure. US is also important in detection of other complications of AVMs, such as bleeding, which may range from asymptomatic anemia to profuse hemorrhage. Furthermore, AVMs may cause steal phenomenon due to arteriovenous shunting and decreased distal tissue perfusion [5]. In the current case, renal arteries were hardly distinguishable during iDSA. Thus, arteriovenous shunting caused a reduction in renal perfusion, which in turn contributed to oliguria and progression of peripheral edema.
In this study, we present for the first time hemodynamically successful embolization of a large retroperitoneal AVM in a very low birth weight neonate. Our report demonstrates that in cases when etiology of pulmonary hypertension cannot be established by ECHO, radiological assessment including brain and abdominal US as well as DSA is needed for establishment of the diagnosis. Prompt initiation of therapy should be warranted as prolonged ischemia could rapidly lead to irreversible dysfunction of vital organs in preterm neonates. In cases when on US there is a strong suspicion for AVM, DSA may be preferred over MRI, as DSA would allow therapeutic intervention in addition to the diagnostic information.
Conflict of Interest
The authors declare no conflict of interest.
Funding
No additional funding was required in the preparation of this case report.
| References | ▴Top |
- Dasgupta R, Fishman SJ. ISSVA classification. Semin Pediatr Surg. 2014;23(4):158-161.
doi pubmed - Jameel A, Amin A, Arif H, Amjad K. Percutaneous coil embolisation of congenital hepatic arteriovenous malformations in two patients with congenital heart disease and review of the literature. Health. 2010;2:906-912.
doi - Thukaram R, Suarez WA, Sundararaghavan S. Transcatheter closure of the patent arterial duct using the Flipper coil in a premature infant weighing 1,400 g: a case report. Catheter Cardiovasc Interv. 2005;66(1):18-20.
doi pubmed - Aly AM, Garcia CY, von Ritschl R. Successful embolization of a large vein of galen malformation in a premature infant presenting with congestive heart failure and persistent pulmonary hypertension. AJP Rep. 2012;2(1):19-22.
doi pubmed - Mulligan PR, Prajapati HJ, Martin LG, Patel TH. Vascular anomalies: classification, imaging characteristics and implications for interventional radiology treatment approaches. Br J Radiol. 2014;87(1035):20130392.
doi pubmed - Soler P, Mehta AV, Garcia OL, Kaiser G, Tamer D. Congenital systemic arteriovenous fistula between the descending aorta, azygos vein, and superior vena cava. Chest. 1981;80(5):647-649.
doi pubmed - Israel PG, Armstrong BE, Effman EL, Newman GE, Anderson PA. Retroperitoneal arteriovenous malformation, a rare cause of heart failure in infancy: consideration of therapeutic approaches. Pediatr Cardiol. 1993;14(1):49-52.
pubmed - Alexander CP, Sood BG, Zilberman MV, Becker C, Bedard MP. Congenital hepatic arteriovenous malformation: an unusual cause of neonatal persistent pulmonary hypertension. J Perinatol. 2006;26(5):316-318.
doi pubmed - Puthiyachirakkal M, Mhanna MJ. Pathophysiology, management, and outcome of persistent pulmonary hypertension of the newborn: a clinical review. Front Pediatr. 2013;1:23.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
