| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website http://www.theijcp.org |
Original Article
Volume 1, Number 1, February 2012, pages 9-18
Clinical Significance of Fever and Leukocytosis in Diagnosis of Acute Appendicitis in Children Who Visit Emergency Department With Abdominal Pain
Sang Hyun Haa, Chong Kun Honga, Younghwan Leea, Ae Jin Sunga, Jun Ho Leea, Kwang Won Choa, Seong Youn Hwanga, Na Kyoung Leea, Hyeon Woo Yimb, c
aDepartments of Emeregncy Medicine and Nursing, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon 630-522, South Korea
bDepartment of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, South Korea
cCorresponding author: Hyeon Woo Yim, Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, 505 Banpo-dong, Seocho-gu, Seoul, 137-701, South Korea
Manuscript accepted for publication January 26, 2012
Short title: Fever and Leukocytosis in Diagnosis
doi: https://doi.org/10.4021/ijcp104e
| Abstract | ▴Top |
Background: The use of fever in the diagnosis of appendicitis in pediatric patients is unproven. The purpose of this investigation was to determine the value of fever in the diagnosis of acute appendicitis in children presenting to the emergency department (ED) with acute abdominal pain.
Methods: Medical records from January-December, 2009, were reviewed for children (age < 18 years) who presented to an ED of one medical center with abdominal pain. Data on initial body temperature, white blood cell count, left shift, and final diagnosis were analyzed.
Results: Of 674 children, 119 had appendicitis. The prevalance of initial fever did not differ between those with and without appendicitis, but the prevalence of leukocytosis and left shift were higher in children diagnosed with appendicitis. Despite of stratification by age, leukocytosis, prevalence of fever was not differing.
Conclusions: Fever does not help in diagnosing appendicitis in our patients. Leukocytosis and white cell left shifts are on the other hand more common in patients with appendicitis. More studies should follow to investigate their role in diagnosis of appendicitis in patients in emergency department.
Keywords: Fever; White blood cell count; Appendicitis ADDIN
| Introduction | ▴Top |
Acute abdominal pain is one of the most common complaints in patients who visit the emergency department (ED). When a patient complains of pain in the right lower quadrant of the abdomen, a clinician faces the challenge of considering acute appendicitis as a possibility [1]. In Korea and internationally, acute appendicitis is one of the most common causes of acute abdominal pain requiring surgical intervention [1]. In cases of delayed diagnosis or misdiagnosis, possible complications including abscess, peritonitis, sepsis, intestinal obstruction and, ultimately, death, may occur [2]. Early diagnosis and treatment of acute appendicitis is crucial. However, the diagnosis is still somewhat difficult from the clinician’s point of view, especially for children. This is because acute appendicitis in children presents symptoms that are often similar to symptoms of illnesses, such as acute gastroenteritis, urinary tract infection, or fecal impaction. Furthermore, communication difficulties related to the young age of a pediatric patient can make a diagnosis more time-consuming and difficult, compared to adults [3]. A misdiagnosis rate of 28% - 57% has been reported in children ≤ 12-years-of-age [3-7].
The Alvarado score for differential diagnosis of acute appendicitis by clinical characteristics and pediatric appendicitis score for pediatric patients have been reported and their diagnostic validities verified [8-11]. Fever and leukocytosis are included in both scoring systems, and several reports have indicated that the presence of fever is indicative of acute appendicitis [6, 12, 13]. However, in another study, in adults diagnosed with acute appendicitis, 15.6% had no fever or leukocytosis [14]. Furthermore, in a study of pediatric patients ≤ 6-years-of-age who visited the ED with abdominal pain, no significant difference in the frequency of fever was evident between patients diagnosed with acute appendicitis and patients who were not [3].
We conducted this study to ascertain if the presence of fever and leukocytosis are indicative factors in the diagnosis of acute appendicitis in children who visit the ED with abdominal pain.
| Materials and Methods | ▴Top |
Subjects
This study used data from a regional emergency medical center visited by approximately 30,000 patients annually. We retrospectively investigated medical records of patients aged ≤ 18-years-of-age who visited the ED from January 1 to December 31, 2009, with the initial chief symptom of abdominal pain (coded as C0000737, following questioning by the attending ED nurse). Because vague abdominal complaints predominates in children than adults, we intended to included all abdominal pain in addition to specific right quadrant pain. This study was approved by the hospital’s Clinical Study Ethics Committee (IRB No. 2010- SCMC-020-00).
Methods
Patient records were excluded if the possibility of acute appendicitis had been ruled out, according to the following criteria: 1) past history of appendectomy, 2) abdominal pain occurring after trauma, 3) abdominal pain related to delivery, and 4) abdominal pain after foreign body ingestion. One investigator submitted the data in a pre-established computerized format. In cases of hospitalized patients, or in patients who visited the ED from an outpatient clinic, we also examined the admission records and outpatient clinic records, respectively. If the data from the ED, admission, and outpatient clinic records differed, the ED records were selected for analysis. Records from a total of 765 patients were initially enrolled. Exclusions were made based on the following: past history of appendectomy (n = 18), abdominal pain occurring post-trauma (n = 9), abdominal pain related to delivery (n = 2), abdominal pain after foreign body ingestion (n = 1), and 12 patients for whom ED medical records were not made. To strengthen the accuracy of final diagnosis, we conducted telephone follow-ups with 329 patients who had not been hospitalized in our hospital or who did not have pathological examination results. We investigated any recurrence of symptom within 1 month after discharge from the ED or if other diagnoses had been made by different medical institutions. Further exclusions are made for 49 patients who either refused to answer the phone survey questions or could not be contacted by calling twice within a 3-day interval. One hundred nineteen patients had a diagnosis of acute appendicitis in their medical records (appendicitis group) and, with the exclusion of aforementioned patients, 329 patients were not diagnosed with appendicitis (Fig. 1). While acute appendicitis has been treated using only antibiotics [15], we assumed that acute appendicitis causes pain in the majority of cases and that the situation cannot be healed naturally. We conducted this study using data from 674 patients and investigated age, sex, initial body temperature, white blood cell (WBC) count, discharge diagnosis recorded in ED or in the ward, pathological examination results, abdomen computed tomography (CT) or ultrasound results. Blood tests are done using a model XE-2100 apparatus (Sysmex, Kobe, Japan) and body temperature was measured at the axilla using a model MT 200 thermometer (Microlife, Basel, Switzerland) during the period of study in our ED.
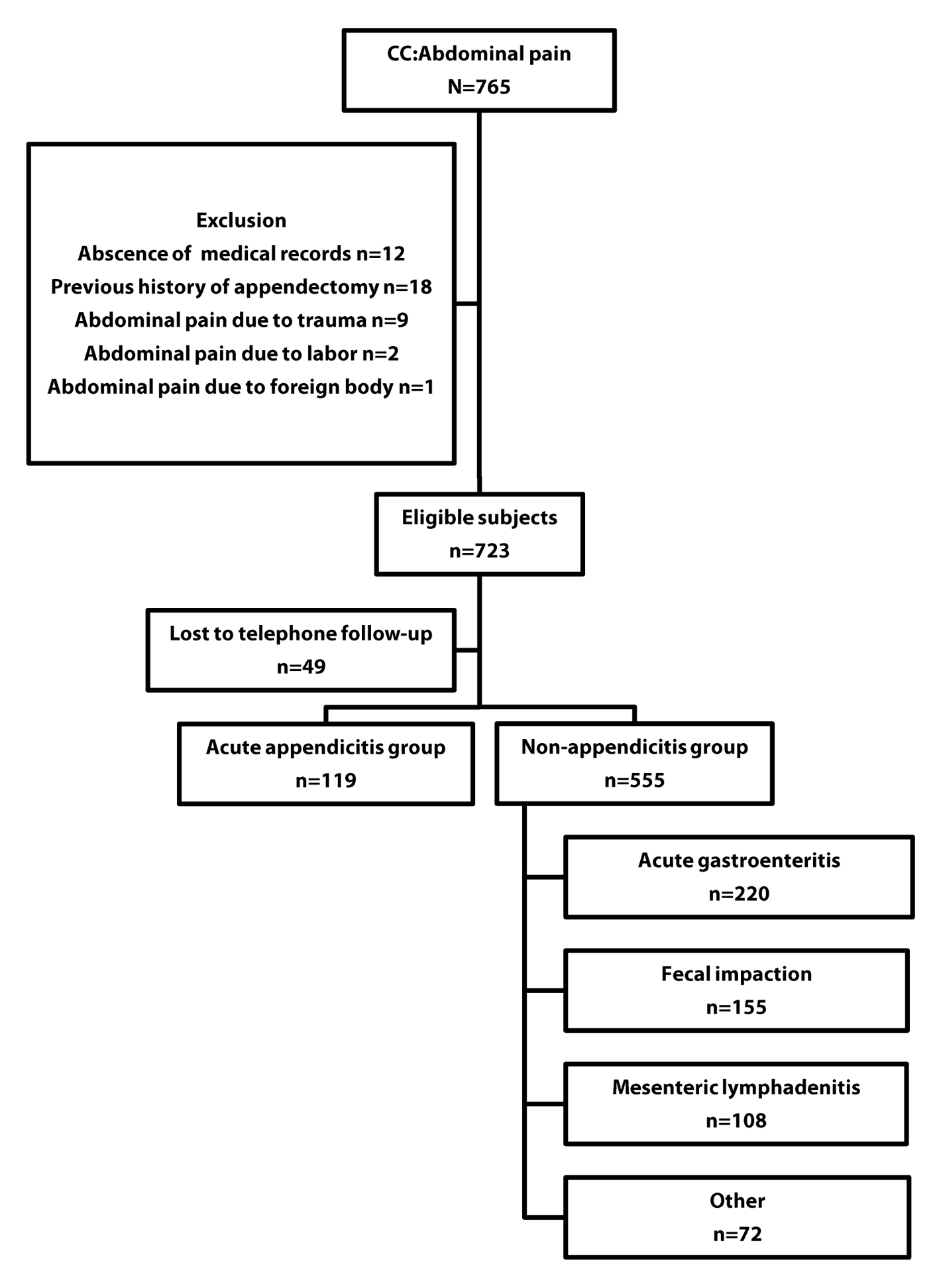 Click for large image | Figure 1. Flow chart of patients with appendicitis. |
Definitions of study variables and outcomes
Acute appendicitis group refers to patients with confirmed acute appendicitis by pathological examination of the specimen. Mesenteric lymphadenitis group refers to patients without evidence of acute appendicitis as detected by abdominal CT or abdominal ultrasound, other than enlargement of mesenteric lymph nodes. Acute gastroenteritis group refers to patients with a recorded final diagnosis by the physician-in-charge and no relapse after discharge and no other diagnosis made by different, or the same medical institution, as revealed in telephone follow ups. Fecal impaction group refers to patients with a recorded final diagnosis by the physician-in-charge, with improvement of symptoms after enema, as recorded in a nursing chart, and no relapse after discharge or other diagnosis made by different, or the same medical institution, as revealed in telephone follow ups. Other groups refer to patients not included in the previous categories. Non-appendicitis group refers to patients in the mesenteric lymphadenitis, acute gastroenteritis, fecal impaction, and other group categories. Body temperature refers to axillary temperature measured and recorded by the ED nurse upon patient presentation at the ED. Fever refers to a body temperature above 37.4 °C [16]. WBC count refers to the first WBC count measured after entering the ED. Shift of WBC to the left (or left shift) refers to the ratio of segmented neutrophil and band form 75% or above, in the first WBC count measured after entering the ED.
Analyses
For final diagnosis, we used pathological diagnosis if a patient had an operation in our hospital and, thus, had a pathological examination of the removed specimen. In other cases, we used the diagnosis made by the attending doctors when the patients were discharged from an ED or a ward. For patients discharged from an ED, we used an ED discharge diagnosis as the final diagnosis if symptoms did not recur or no different diagnosis made by other medical institution, as checked by our telephone follow-ups. We divided 674 patients into the acute appendicitis and non-acute appendicitis groups, and compared the frequency of fever as an initial presenting symptom. Because of the difference between the body temperature and rectal temperature, we used 37.4 °C or higher, to make it comparable to fevers in other studies that defined fever as body temperature ≥ 38 °C [16]. Also, we compared the frequency of leukocytosis between the groups using a WBC standard of > 10,000 cells/mm, consistent with most studies [3, 17-20]. Lastly, to compensate for the effect of change in leukocyte levels, shift of WBC to the left and age on the temperature, we stratified each of these factors and used receiver operating characteristic (ROC) curve analysis to analyze diagnostic significance of fever (≥ 37.4 °C). Statistical analysis was performed by PASW ver. 18.0 (SPSS, Chicago, IL). Two sample T-test was used for continuous data and was converted into categorical data when needed, followed by Chi-squared test. Statistical significance was defined at P < 0.05.
| Results | ▴Top |
Characteristics of the study population
Seven hundred and sixty five patients visited our emergency center during the 1-year period of data collection. Data from 674 patients was used. One hundred nineteen patients were diagnosed with acute appendicitis, and 555 of them were not (Fig. 1). We were able to acquire WBC level data in all 119 patients from the acute appendicitis group and 398 of 555 patients in the non-acute appendicitis group.
No difference in sex was found between the groups. However, the acute appendicitis group had more aged patients. Initial body temperatures first measured after entering an ED did not differ significantly between the groups. Fever (≥ 37.4 °C) was evident in 11.8% and 13.7% of patients in the acute appendicitis and non-appendicitis group, respectively, and the difference was not significant (Table 1). We categorized the patients into three age groups: 1 - 3, 4 - 11, and 12 - 18 years. No age-related significant differences were evident (Table 2).
 Click to view | Table 1. Comparison of Characteristics of Study Population |
 Click to view | Table 2. Comparison of Fever and White Blood Cell Between Appendicitis and Non-Appendicitis Stratified by Age |
WBC levels obtained from 517 of the 674 patients were analyzed using two samples T-test. The WBC level in the acute appendicitis group (14,800/mm3) was significantly higher than in the non-appendicitis group (9,700/mm3). Defining WBC level ≥10,000/mm3 as leukocytosis, results of χ2 test showed a significantly higher frequency of leukocytosis in the acute appendicitis group (Table 1). In the age-stratified analysis, all patients in the acute appendicitis group showed significantly high frequency of leukocytosis, except for ≤ 3-years-of-age (Table 2).
The segment neutrophil ratio in both groups was analyzed using two samples T-test; the 78.6% of the acute appendicitis group was significantly higher than the 64.4% of the non-appendicitis group (Table 1).
Defining the left shift of WBC as ≥ 75%, the results of χ2 test showed significantly high frequency of the left shift of WBC in the acute appendicitis group (Table 1). In the age-stratified analysis, all in the acute appendicitis group showed significantly high frequency of the left shift of WBC, except for patients ≤ 3-years-of-age (Table 2).
We categorized the patients in the non-appendicitis group into four subgroups, according to their final diagnosis (i.e., acute gastroenteritis group, fecal impaction group, mesenteric lymphadenitis group, and other). Other included abdominal pain due to ovarian cyst (n = 8), urolithiasis (n = 4), nonspecific abdominal pain (n = 5), and acute upper respiratory tract infection (n = 8). The fecal impaction group had significantly lower age. No significant differences in sex and initial body temperature were found in the four groups. WBC level and segment neutrophil ratio were significantly high in patients in the ‘other’ group (Table 3).
 Click to view | Table 3. Comparison of Characteristics of Non-Appendicitis Group |
Significance of initial body temperature, WBC level, and left shift of WBC on diagnosis of acute appendicitis, and ROC curve analysis
Initial body temperature, WBC level, and left shift of WBC were analyzed using ROC curve to find out their diagnostic significance. Initial body temperature was insignificant in the diagnosis of acute appendicitis (Fig. 2A). However, the WBC level (Fig. 2B) and the segment neutrophil ratio (Fig. 2C) showed an area-under the curve value of 0.815 and 0.766, respectively, implying a diagnostic value.
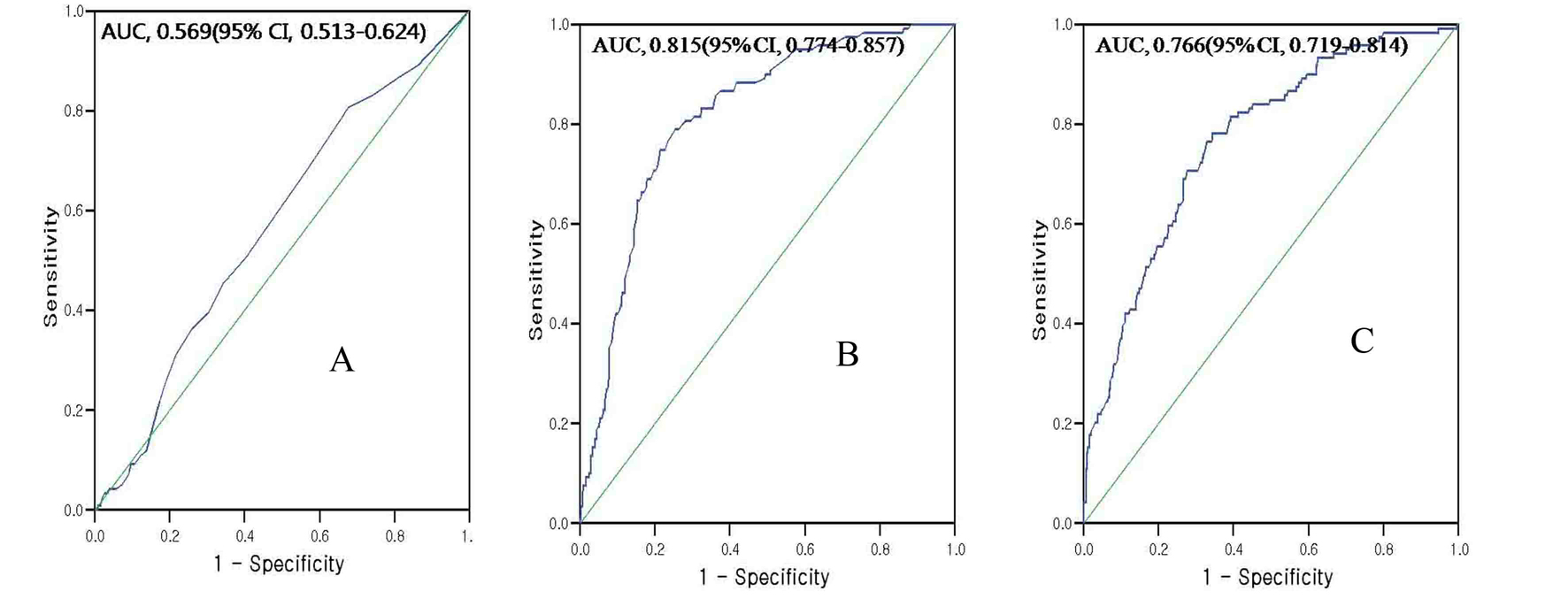 Click for large image | Figure 2. ROC points and fitted AUCs for the acute appendicitis. ROC points and fitted AUCs for fever for the acute appendicitis (A), ROC points and fitted AUCs for WBC count for the acute appendicitis (B), ROC points and fitted AUCs for segment neutrophil for the acute appendicitis (C). |
Significance of initial body temperature on diagnosis of acute appendicitis: stratified ROC curve analysis
The significance of initial body temperature on diagnosis of acute appendicitis was analyzed using ROC curve and using the following stratified factors: WBC level of 10,000/mm3 [17-20] (and higher or lower), segment neutrophil ratio of 75% (and higher or lower), and age. Patients with WBC level ≥ 10,000/mm3 were analyzed using ROC curve; the results indicated that body temperature had no diagnostic value. Similar results were found when the patients with WBC level < 10,000/mm3 were analyzed using ROC curve (Fig. 3A, B). In analyses of stratified factors of segment neutrophil ratio, no diagnostic value of body temperature was evident (Fig. 3C, D). In the age-stratified analysis, all three groups showed no diagnostic value of body temperature (Fig. 3E, F, G). When we specifically extracted the mesenteric lymphadenitis group (mesenteric lymphadenitis is an illness that is difficult to differentiate from acute appendicitis), and compared it to the acute appendicitis group, body temperature was not useful in differentiating the two illnesses (Fig. 3H).
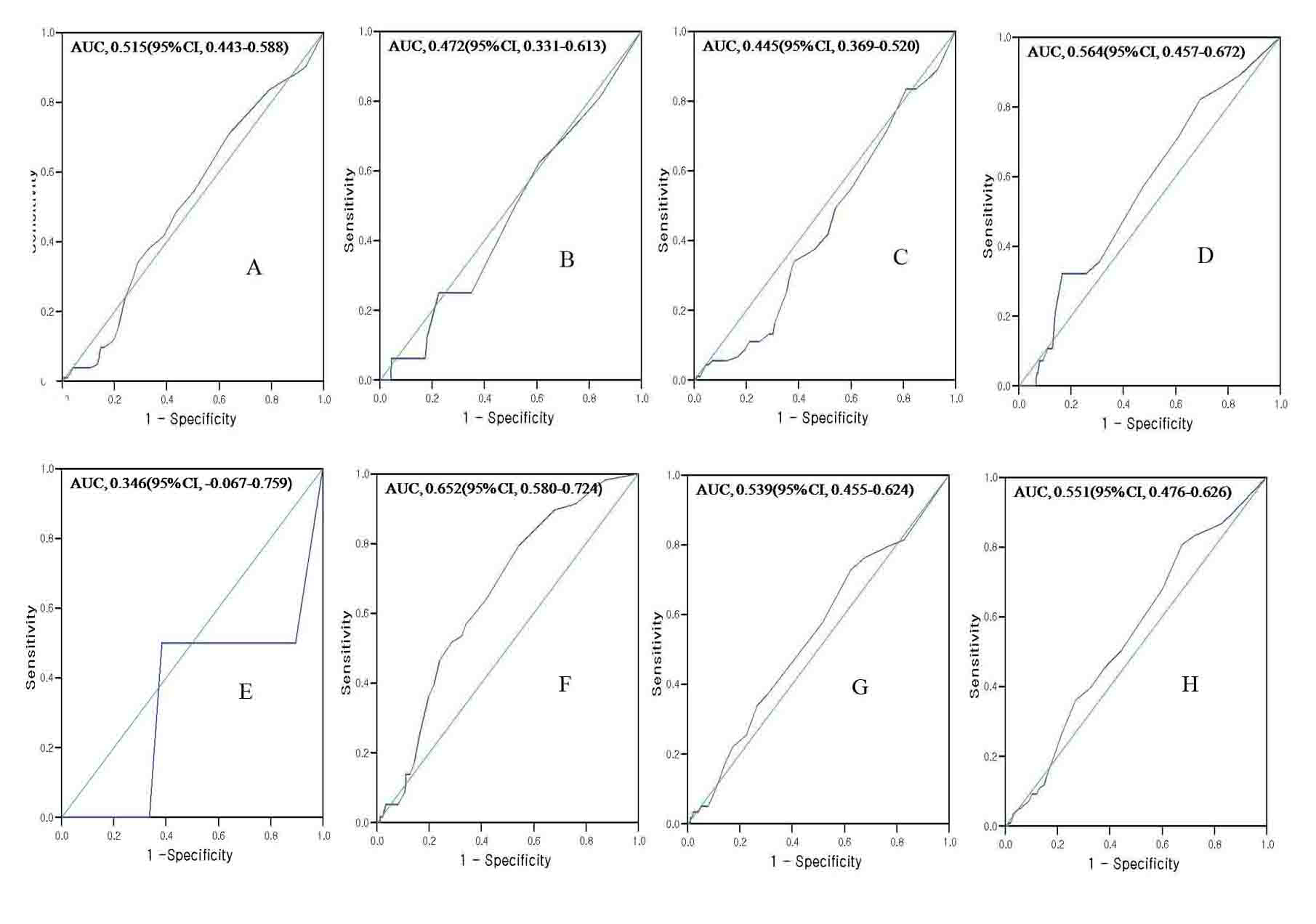 Click for large image | Figure 3. ROC points and fitted AUCs for fever for the acute appendicitis. Study population with WBC count over 10,000/mm3 (A), Study population with WBC count under 10,000/mm3 (B), Study population with segment neutrophil over 75% (C), Study population with segment neutrophil under 75% (D), Study population with age range 1 - 3 years (E), Study population with age range 4 - 11 years (F), Study population with age range over 12 years (G). Among study population, acute appendicitis and mesenteric lymphadenitis (H). |
| Discussion | ▴Top |
Early diagnosis of acute appendicitis in pediatric patients remains difficult, even for an experienced clinician. The diagnostic approaches of two scoring systems [10, 21] have been verified as being useful in diagnosis [8, 9]. However, the diagnostic value of fever or leukocytosis is debatable [3, 6, 12-14, 21]. Monneuse et al. analyzed 326 patients suspected of acute appendicitis prior to surgical intervention and reported that fever or leukocytosis was not detected in 15.6% of the patients [14]. The authors suggested that fever and leukocytosis cannot be reliably used to rule out acute appendicitis. Coleman et al. categorized acute appendicitis patients into four groups (acute, necrotic, abscess-forming, and peritonitis-forming) and reported no difference in frequency of leukocytosis [21]. In addition, the authors categorized all the acute appendicitis patients into a leukocytosis group and non-leukocytosis group; no difference in body temperature between the groups was found.
In contrast, Wang et al. studied patients who visited the ED with a chief complaint of abdominal pain, and reported that in cases of co-existing leukocytosis and left shift of WBC, the sensitivity and specificity of diagnosis of acute appendicitis was 79% and 80%, respectively, evidence that leukocytosis is an indicative finding of acute appendicitis[22].
In this study, we retrospectively investigated medical records of 765 patients aged ≤ 18-years-of-age who visited one emergency center during a 1-year period with initial chief symptom of abdominal pain, with the aim of clarifying the diagnostic value of fever in acute appendicitis. We compared 119 patients with a final diagnosis of acute appendicitis with 555 patients not diagnosed with the illness.
The age of the acute appendicitis group was higher than the non-acute appendicitis group. We assume this is because we included children of all pediatric ages, from 1 - 18 years, and the fact that the frequency of acute appendicitis is relatively low in children aged ≤ 3 years. Among the 119 acute appendicitis patients, only two were ≤ 3-years-of-age (1.6%), similar to result reported by Alloo et al.[6].
In this study, the definition of fever obtained by axillary measurement, consistent with the norm, was ≥ 37.4 °C [17, 20]. Lin et al. reported that an acute appendicitis group had higher frequency of fever in comparison to a non-appendicitis group (43.4% and 17%, respectively) in a study of pediatric patients who visited the ED with abdominal pain in the right lower quadrant [13]. However, in this study, the average body temperature in the acute appendicitis group and non-appendicitis group was 36.8 °C and 36.6 °C, respectively, which was statistically insignificant. Colvin et al. also reported similar results, in which body temperatures in both groups were the same, at 37.4 °C at the time of admission to the ED, similar to the assertion that the initial body temperature does not aid in differential diagnosis of acute appendicitis [3]. When the acute appendicitis and non-appendicitis patients were grouped into two according to presence or absence of fever, then compared with each other, the frequencies of fever were 11.8% and 13.7%, respectively, and the difference was not significant. A similar result was found in the age-stratified analysis of the groups. This is similar to the report of Colvin et al., in which an age-stratified analysis of the group withfever ≥ (38 °C) and the group which had not, and reported no difference in all the age groups [3].
The majority of studies [6, 13, 22, 23] assert that an increase in WBC level indicates acute appendicitis. A similar result was found in our study. In the acute appendicitis group, the average WBC level was 14,800/mm3, which was higher than the 9,700/mm3 of the non-acute appendicitis group. The segment neutrophil ratio was also higher in the acute appendicitis group. In age-stratified analysis, only the age group of ≤ 3 years did not show difference in frequency of leukocytosis and frequency of the left shift of WBC. But, only two patients were aged under 3 in our study, making if imprudent to generalized our finding. However, it is relevant that Paajanen et al. also reported a weak inflammatory reaction in response to acute appendicitis in infants and, hence, a feeble increase in WBC level [24].
To investigate the diagnostic value of body temperature and to eliminate confusion derived from factors such as WBC level, we stratified each factor then conducted ROC curve analysis, which showed insignificance in most cases. In the 4 - 11 year-old age group, however, the analysis did reveal the diagnostic significance of fever. But, when the area under the curve of 0.652 was applied alone, its diagnostic value seemed feeble.
When we specifically compared the mesenteric lymphadenitis group (a non-acute appendicitis group) to the acute appendicitis group, the results showed that body temperature was not helpful in differentiating the two illnesses.
Characteristics, as well as limitations, of this study are as follows. Firstly, we investigated all patients who visited a single hospital with abdominal pain, hence there was no selection bias. The percentage of patients diagnosed with acute appendicitis among those who came to the hospital with abdominal pain was 17.7%, which is considered high. This is because, as a tertiary medical institution, our hospital has many referrals of patients suspected of having acute appendicitis from primary and secondary medical institutions, which explains the higher frequency of patients requiring surgical intervention among those who came to the hospital with abdominal pain. As such, the results from this study may not be applicable to the circumstances in primary and secondary medical institutions. Among the 119 patients, there were only two patients between the ages of 1 and 3.9 years who were analyzed. It is well-known that fewer than 5% of patients diagnosed with appendicitis are ≤ 4-years-of-age. Our results are consistent with these findings, but the small number of patients in this age group makes any conclusions from the present data impossible. For this reason, a long-term, prospective, observational cohort study is needed.
Secondly, this study was a retrospective, cross-sectional study that was based on medical records. Hence, the possibility of measurement error and erroneous data may exist, and there is the possibility that bias may have intervened during data collection. To minimized bias in this study, we only used body temperature and WBC level, which are objective indices. To strengthen the final diagnosis of patients with abdominal pain, we conducted telephone follow-ups with those who had been discharged from the ED, in an attempt to minimize measurement error.
Thirdly, as one of limitations of a retrospective, cross-sectional study, administration of an antipyretic prior to visiting ED was not recorded in the charts, so we could not check any possible effect of antipyretic administration. However, in our study, the initial body temperature was not diagnostically important in diagnosis of acute appendicitis in patients found in emergency settings.
In conclusion, in patients ≤ 18-years-of-age who visited the ED with the chief complaint of abdominal pain, no difference in frequency of fever was found between the acute appendicitis group and non-acute appendicitis group. Fever does not help in diagnosing appendicitis in our patients. But leukocytosis and white cell left shifts are on the other hand more common in patients with appendicitis. More studies should follow to investigate their role in diagnosis of appendicitis in patients in emergency department.
Acknowledgments
There is no financial support from any institutes and the authors individually or collectively have no significant financial conflicts that need disclosing.
Conflict of Interest Statement
The authors have no conflict of interests and no financial disclosures.
| References | ▴Top |
- Lee JH, Park YS, Choi JS. The epidemiology of appendicitis and appendectomy in South Korea: national registry data. J Epidemiol. 2010;20(2):97-105.
pubmed doi - Rothrock SG, Pagane J. Acute appendicitis in children: emergency department diagnosis and management. Ann Emerg Med. 2000;36(1):39-51.
pubmed doi - Colvin JM, Bachur R, Kharbanda A. The presentation of appendicitis in preadolescent children. Pediatr Emerg Care. 2007;23(12):849-855.
pubmed doi - Rothrock SG, Skeoch G, Rush JJ, Johnson NE. Clinical features of misdiagnosed appendicitis in children. Ann Emerg Med. 1991;20(1):45-50.
pubmed doi - Nance ML, Adamson WT, Hedrick HL. Appendicitis in the young child: a continuing diagnostic challenge. Pediatr Emerg Care. 2000;16(3):160-162.
pubmed doi - Alloo J, Gerstle T, Shilyansky J, Ein SH. Appendicitis in children less than 3 years of age: a 28-year review. Pediatr Surg Int. 2004;19(12):777-779.
pubmed doi - Paajanen H, Somppi E. Early childhood appendicitis is still a difficult diagnosis. Acta Paediatr. 1996;85(4):459-462.
pubmed doi - Goldman RD, Carter S, Stephens D, Antoon R, Mounstephen W, Langer JC. Prospective validation of the pediatric appendicitis score. J Pediatr. 2008;153(2):278-282.
pubmed doi - Bhatt M, Joseph L, Ducharme FM, Dougherty G, McGillivray D. Prospective validation of the pediatric appendicitis score in a Canadian pediatric emergency department. Acad Emerg Med. 2009;16(7):591-596.
pubmed doi - Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557-564.
pubmed doi - Kharbanda AB, Taylor GA, Fishman SJ, Bachur RG. A clinical decision rule to identify children at low risk for appendicitis. Pediatrics. 2005;116(3):709-716.
pubmed doi - Graham JM, Pokorny WJ, Harberg FJ. Acute appendicitis in preschool age children. Am J Surg. 1980;139(2):247-250.
pubmed doi - Lin CH, Chen JH, Li TC, Ho YJ, Lin WC. Children presenting at the emergency department with right lower quadrant pain. Kaohsiung J Med Sci. 2009;25(1):1-9.
pubmed doi - Monneuse O, Abdalla S, Pilleul F, Hervieu V, Gruner L, Tissot E, Barth X. Pain as the only consistent sign of acute appendicitis: lack of inflammatory signs does not exclude the diagnosis. World J Surg. 2010;34(2):210-215.
pubmed doi - Mason RJ. Surgery for appendicitis: is it necessary? Surg Infect (Larchmt). 2008;9(4):481-488.
pubmed doi - Temperature measurement in paediatrics. Paediatr Child Health. 2000;5(5):273-284.
pubmed - Pearl RH, Hale DA, Molloy M, Schutt DC, Jaques DP. Pediatric appendectomy. J Pediatr Surg. 1995;30(2):173-178; discussion 178-181.
pubmed doi - Wu HP, Chang CF, Lin CY. Predictive inflammatory parameters in the diagnosis of acute appendicitis in children. Acta Paediatr Taiwan. 2003;44(4):227-231.
pubmed - Harland RN. Diagnosis of appendicitis in childhood. J R Coll Surg Edinb. 1991;36(2):89-90.
pubmed - van den Broek WT, van der Ende ED, Bijnen AB, Breslau PJ, Gouma DJ. Which children could benefit from additional diagnostic tools in case of suspected appendicitis? J Pediatr Surg. 2004;39(4):570-574.
pubmed doi - Coleman C, Thompson JE, Jr., Bennion RS, Schmit PJ. White blood cell count is a poor predictor of severity of disease in the diagnosis of appendicitis. Am Surg. 1998;64(10):983-985.
pubmed - Wang LT, Prentiss KA, Simon JZ, Doody DP, Ryan DP. The use of white blood cell count and left shift in the diagnosis of appendicitis in children. Pediatr Emerg Care. 2007;23(2):69-76.
pubmed doi - Ng KC, Lai SW. Clinical analysis of the related factors in acute appendicitis. Yale J Biol Med. 2002;75(1):41-45.
pubmed - Paajanen H, Mansikka A, Laato M, Kettunen J, Kostiainen S. Are serum inflammatory markers age dependent in acute appendicitis? J Am Coll Surg. 1997;184(3):303-308.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
