| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website https://www.theijcp.org |
Case Report
Volume 12, Number 1, May 2023, pages 15-21
Foot Drop Following Epidural Catheter Placement for Postoperative Analgesia Following Lower Extremity Orthopedic Surgery in an Adolescent: Investigation and Etiology
Amr Elhamrawya, c, Joseph D. Tobiasa, b, Giorgio Venezianoa, b
aDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
bDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
cCorresponding Author: Amr Elhamrawy, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted April 10, 2023, accepted April 26, 2023, published online May 4, 2023
Short title: Foot Drop and Epidural Analgesia
doi: https://doi.org/10.14740/ijcp513
| Abstract | ▴Top |
Although the incidence of significant neurologic injury following epidural analgesia remains exceedingly low in both adult and pediatric patients, the consequences of such injury can be devasting. Given these concerns, immediate investigation into the etiology of postoperative neurologic deficits is mandatory, especially when they occur in the dermatomes affected by the neuraxial technique. We report an 18-year-old male patient who had an intraoperative lumbar epidural catheter placed to provide analgesia following lower extremity oncologic surgery. Foot drop was noted on the fourth postoperative day. Potential etiologies for this neurologic deficit are presented, appropriate workup discussed, and previous anecdotal reports of similar occurrences reviewed.
Keywords: Common peroneal nerve; Foot drop; Neuropraxia; Epidural hematoma
| Introduction | ▴Top |
Given its potential benefits and the limited risk of significant adverse effects, neuraxial anesthesia remains a frequently chosen option for both intraoperative anesthetic care as well as the provision of postoperative analgesia [1-3]. In addition to its analgesic benefits, which may exceed those of systemic opioid administration, epidural anesthesia effectively blunts the physiological and metabolic impact associated with tissue injury and surgical procedures [4]. This is especially true following lengthy and complex procedures which may result in activation of the sympathetic nervous system, leading to the release of inflammatory mediators including interlukin-6, interlukin-1, and tumor necrosis factor-alpha [4].
Although the incidence of significant neurologic injury such as epidural hematoma formation, radiculopathy, direct spinal cord injury, and cauda equina syndrome following neuraxial anesthesia remains exceedingly low in both adult and pediatric patients, the consequences of such injury can be devasting [5-11]. Given these concerns, immediate investigation into the etiology of postoperative neurologic deficits is mandatory, especially when they occur in the dermatomes affected by the neuraxial technique. We report an 18-year-old male patient who had an intraoperative lumbar epidural catheter placed to provide intraoperative and postoperative analgesia following lower extremity oncologic surgery. He subsequently was noted to have foot drop on the fourth postoperative day (POD). The presence of any neurologic deficit in a patient with an indwelling epidural catheter may signal the presence of a surgical emergency (epidural hematoma formation). Given the potential for permanent spinal cord damage with paralysis if emergent surgical decompression is not performed, a formalized and rapid approach to investigate and diagnose the etiology including emergent magnetic resonance imaging (MRI) is needed. Potential etiologies for this neurologic deficit are presented, appropriate workup discussed, and previous anecdotal reports of similar occurrences reviewed.
| Case Report | ▴Top |
Review of this case and presentation in this format followed the guidelines of the Institutional Review Board approval at Nationwide Children’s Hospital (Columbus, Ohio). An 18-year-old, 80.9 kg, American Society of Anesthesiologists’ physical status (ASA) III adolescent with a history of Ewing’s sarcoma presented for right femur fixation, right hardware removal, and application of a microvascular free fibular graft to the upper leg for bony reconstruction of the extremity. Past surgical history was remarkable for adenotonsillectomy at 5 years of age, previous right femur tumor resection at 15 years of age for the primary occurrence of Ewing’s sarcoma, insertion of an implanted central venous port, and right thoracoscopy with resection of a pulmonary nodule. There was no history of surgical concerns. His family history was unremarkable. The patient denied alcohol, tobacco or illicit substance use. Current medications included sulfamethoxazole (800 mg by mouth twice a day, 2 days a week), loperamide (2 mg tablet as needed), escitalopram (20 mg by mouth once a day), cefdinir (300 mg tablet twice a day), pantoprazole (40 mg once a day) and buspirone (5 mg twice a day). Preoperative physical examination revealed an adolescent in no acute distress. Airway, cardiac and respiratory examination were within normal limits. Preoperative laboratory evaluation including a complete blood count, coagulation profile, electrolytes, and renal function was normal. The hemoglobin was 11.7 g/dL with a hematocrit of 34.6%. The patient was held nil per os for 8 h and was transported to operating room where routine American Society of Anesthesiologists’ monitors were applied. A peripheral 18-gauge peripheral venous cannula was in place. Midazolam (2 mg) and three doses of fentanyl (total dose of 150 µg) were administered intravenously. The patient was then positioned in the sitting position for lumbar epidural catheter placement. After the skin was cleansed with 2% chlorhexidine, topical and subcutaneous anesthesia was achieved using 1% lidocaine. An 18-gauge Tuohy needle was inserted at the L3-L4 (lumbar) level. After loss of resistance, using a glass syringe filled with normal saline, the epidural catheter was inserted 4 cm into the epidural space. After a negative test dose (3 mL of lidocaine 1.5% with epinephrine 1:200,000), 10 mL of 0.2% ropivacaine was administered followed by an infusion of 0.2% ropivacaine with clonidine (1 µg/mL) at 8 mL/h. Anesthesia was induced with propofol (250 mg) and fentanyl (25 µg). Bag-valve-mask ventilation was provided without difficulty and neuromuscular blockade was achieved with rocuronium (50 mg). The patient’s trachea was intubated with 7.0 mm cuffed endotracheal tube on the first attempt using a Macintosh 3 laryngoscope blade and direct laryngoscopy. After the induction of anesthesia, a second peripheral intravenous cannula was placed, and an arterial cannula was inserted into the left radial artery using ultrasound guidance. Maintenance anesthesia included sevoflurane (expired concentration 2-4%) in air and oxygen and hydromorphone (total dose of 1 mg at the start of the procedure). Neuromuscular blockade was provided by intermittent doses of rocuronium. Cefazolin (2 g) was administered every 3 h for prophylaxis against surgical site infections. The procedure lasted approximately 17 h with the patient in the supine position. Heart rate was maintained between 70 and 90 beats per minute with a normal sinus rhythm and mean arterial pressure was maintained also to be between 60 and 80 mm Hg. Total fluid intake was approximately 7,000 mL including lactated Ringers (3 L), normal saline (1.5 L), 5% albumin (2 L), and one unit of allogeneic packed red blood cells. Total output included urine (2,050 mL) and an estimated blood loss of 400 mL. At the end of the procedure, ondansetron (4 mg) was administered as a prophylaxis of postoperative nausea and vomiting, and residual neuromuscular blockade was reversed with sugammadex (200 mg). His trachea was extubated when awake. He was transferred to the post-anesthesia care unit and then admitted to the inpatient ward. Initial assessment by the acute pain service revealed adequate pain control and stable vital signs with a pulse of 108 beats/min, blood pressure of 120/59 mm Hg, temperature of 37.2 °C, and room air oxygen saturation of 98%. On POD 1, the patient complained of pain on the lateral aspect of the right ankle (surgical side) which was not covered by the lumbar placed epidural. This was attributed to missed sacral coverage by the epidural infusion. The pain was treated with systemic medications (oral and intravenous). On POD 3, the epidural infusion was discontinued, and the catheter removed. On POD 4, the nurse noticed slight weakness of the left lower extremity (contralateral side to the surgical procedure). On the following day, the patient was still complaining of weakness especially dorsiflexion of the left ankle with decreased sensation of the entire left forefoot. Given the presence of the neurologic deficit, neurosurgery was consulted. MRI was obtained to rule out epidural hematoma or spinal cord injury. MRI of the spine was unremarkable for spinal cord injury or any identifiable etiology of foot drop. On POD 8, MRI of the left lower extremity demonstrated abnormal T2 bright signal in the common peroneal nerve and the proximal tibial nerve along its course around the fibular head and neck. There was no evidence of nerve transection. There was no perineural mass, hemorrhage, or cyst. There was a normal appearance to the sciatic nerve. The radiologic interpretation was left lower extremity common peroneal nerve injury (neuropraxia) due to extrinsic compression neuropathy. The patient was discharged home on POD 9. At that time, he had demonstrated early signs of functional improvement since the initial evaluation with improved strength of both dorsiflexion and foot eversion. His conservative management plan included physical therapy and bracing as needed. Given the presumed mechanism of injury, functional improvement and recovery were expected. At his most recent 3-month follow-up visit, physical examination reveals full inversion of the ankle and toe plantar flexion, 4/5 eversion of the ankle, 2/5 ankle dorsiflexion, and 1/5 toe dorsiflexion. There is improved sensation on the dorsal aspect of the foot and the first dorsal webspace.
| Discussion | ▴Top |
We present an 18-year-old patient who developed a new neurologic deficit (foot drop contralateral to the site of the surgical procedure) on POD 4-5 following a prolonged surgical procedure with use of a lumbar epidural catheter for postoperative analgesia. As the presence of any neurologic deficit in a patient with an ongoing or a recent history of an indwelling epidural catheter may signal the presence of a surgical emergency (epidural hematoma formation), a formalized and rapid approach to investigate and diagnose the etiology is recommended. The presence of any neurologic deficit or suspected injury in a patient with a recent or ongoing indwelling epidural catheter should be viewed as a medical emergency with the need for immediate evaluation and physical examination to document the extent of the neurologic deficit, cessation of the epidural infusion followed by emergent MRI to rule out a surgical lesion such as an epidural hematoma. As the MRI of the spinal cord was unremarkable, to further determine the etiology of the neurologic deficit, MR neurography was obtained of the lower extremity. This revealed an abnormal T2 bright signal in the common peroneal nerve and the proximal tibial nerve along its course around the fibular head and neck, suggesting the diagnosis of a peripheral nerve injury from positioning or external compression.
Despite its rarity, epidural hematoma formation can result in permanent and devastating neurologic injury including paralysis. As the potential for progressive neurologic damage remains time-sensitive, early diagnosis and treatment is essential [11, 12]. The potential for devastating neurologic complications is illustrated by a case report of Han et al, who noted the development of postoperative spinal cord compression from an epidural hematoma after epidural anesthesia in an adult patient receiving deep vein thrombosis prophylaxis with enoxaparin following hip arthroplasty [13]. The epidural hematoma was discovered after epidural catheter removal on POD 2 when the patient complained of decreased sensation and movement in the leg on the operative side. The diagnosis was confirmed by MRI; however, no improvement in neurologic function was noted after spinal cord decompression.
Sensory innervation of the lower extremity is provided primarily by branches and nerves from the lumbar and sacral plexuses. The lumbar plexus is formed by the union of the anterior rami of the first four lumbar nerves (L1-4) with variable input from the 12th thoracic nerve (T12) and L5. The lumbar plexus lies in the “psoas compartment” in the paravertebral space with the anterior border formed by the psoas major muscle and the posterior border formed by the quadratus lumborum. As it emerges from this space, it divides into the three nerves that innervate the anterior portion of the upper aspect of the lower extremity: femoral, lateral femoral cutaneous, and obturator nerves. The sacral plexus is formed by the anterior rami of the fourth and fifth lumbar nerves and the first three sacral nerves with variable input from the fourth sacral nerve. The sacral plexus lies on the surface of the sacrum anterior to the piriformis muscle. The sacral plexus gives rise to the other two nerves that innervate the lower extremity: the posterior cutaneous nerve of the thigh otherwise known as the small sciatic nerve and the sciatic nerve. As the sciatic nerve passes posteriorly behind the knee, it divides into the tibial nerve that continues to course posteriorly along the leg (behind the tibia) and the common peroneal nerve (L4-S2). Proximal to the popliteal fossa, the common peroneal nerve separates from the sciatic nerve and courses along the posterolateral aspect of the leg until it passes anteriorly around the head and neck of the fibula (Fig. 1). As it passes around the fibular neck, which is the most sensitive site for nerve compression as shown, it divides into two terminal branches, the superficial and deep fibular nerves. Both the anterior and lateral muscular compartments of the leg are innervated by the common peroneal nerve and its branches. The tibialis anterior muscle, extensor hallucis longus muscle, and extensor digitorum longus muscle are components of the anterior muscular compartment of the leg, which are responsible for foot dorsiflexion. The fibularis longus muscle and fibularis brevis muscle are components of the lateral muscular compartment of the leg, being responsible for foot eversion. As the common peroneal nerve is a mixed nerve, it has both sensory and motor function. The superficial fibular nerve carries sensory innervation to anterolateral aspect of the leg (from middle half of lower leg to the dorsal aspect of foot and toes) except for the space between first and second toes which is supplied by the deep fibular nerve [14].
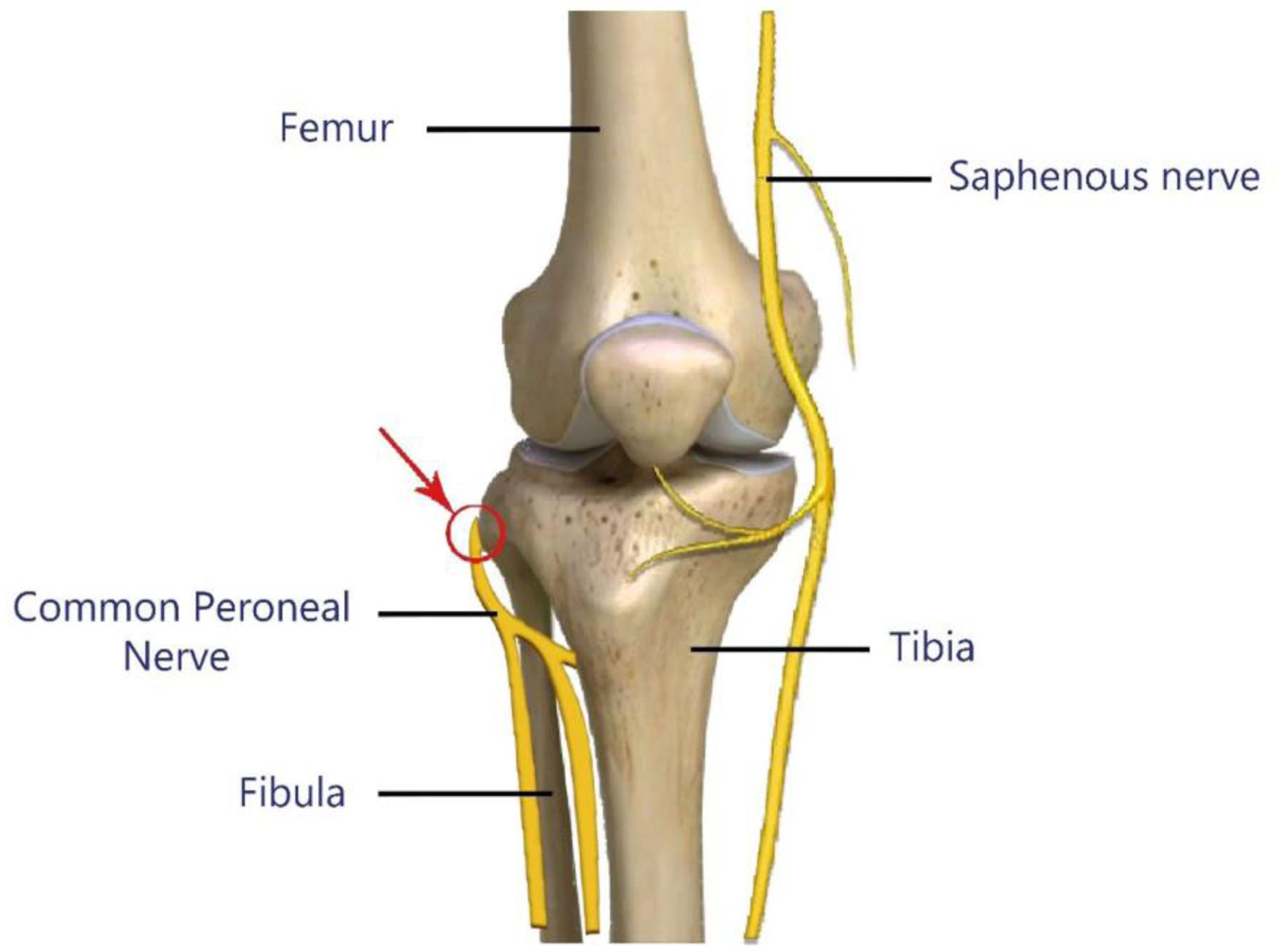 Click for large image | Figure 1. Common site of common peroneal nerve compression during positional injury (arrow and red circle). |
Foot drop is a commonly used term to describe the motor phenomenon or consequence of involvement of the common peroneal nerve and muscles of the anterior compartment of the lower extremity. The term refers to weakness or absence in dorsiflexion of foot and toes at ankle joint. Common peroneal nerve injury results in wide range of symptoms including numbness, paresthesia, and motor deficits. Etiologies of foot drop include three main categories: central nervous system (CNS) involvement (tumor, hemorrhage), spinal nerve root involvement (disc herniation or trauma compressing the L4-5 spinal nerves), and peripheral conditions (involvement of the common peroneal nerve). In our patient, given the presence of an epidural catheter and concerns of spinal cord involvement, immediate MRI was obtained to rule out a surgical emergency such as an epidural hematoma. With that ruled out, MRI of the lower extremity demonstrated a more peripheral lesion likely related to external compression of the common personal nerve.
When considering the etiologies of a peripheral nerve lesion, compression, stretch, and ischemia are the primary mechanisms. As compression is the most common etiology for perioperative foot drop, injury occurs most commonly at the fibular head, given the superficial location of the nerve and the prominence of the fibular head. Various positioning and intraoperative conditions have been reported as potential causes of perioperative common peroneal nerve injury [15-19]. Many of these injuries can be prevented with appropriate positioning and padding of bony prominences and pressure points in contact with the operating table (Figs. 2 and 3). To date, there are a limited number of anecdotal reports regarding foot drop occurring postoperatively in patients receiving neuraxial anesthesia (Table 1) [20-27].
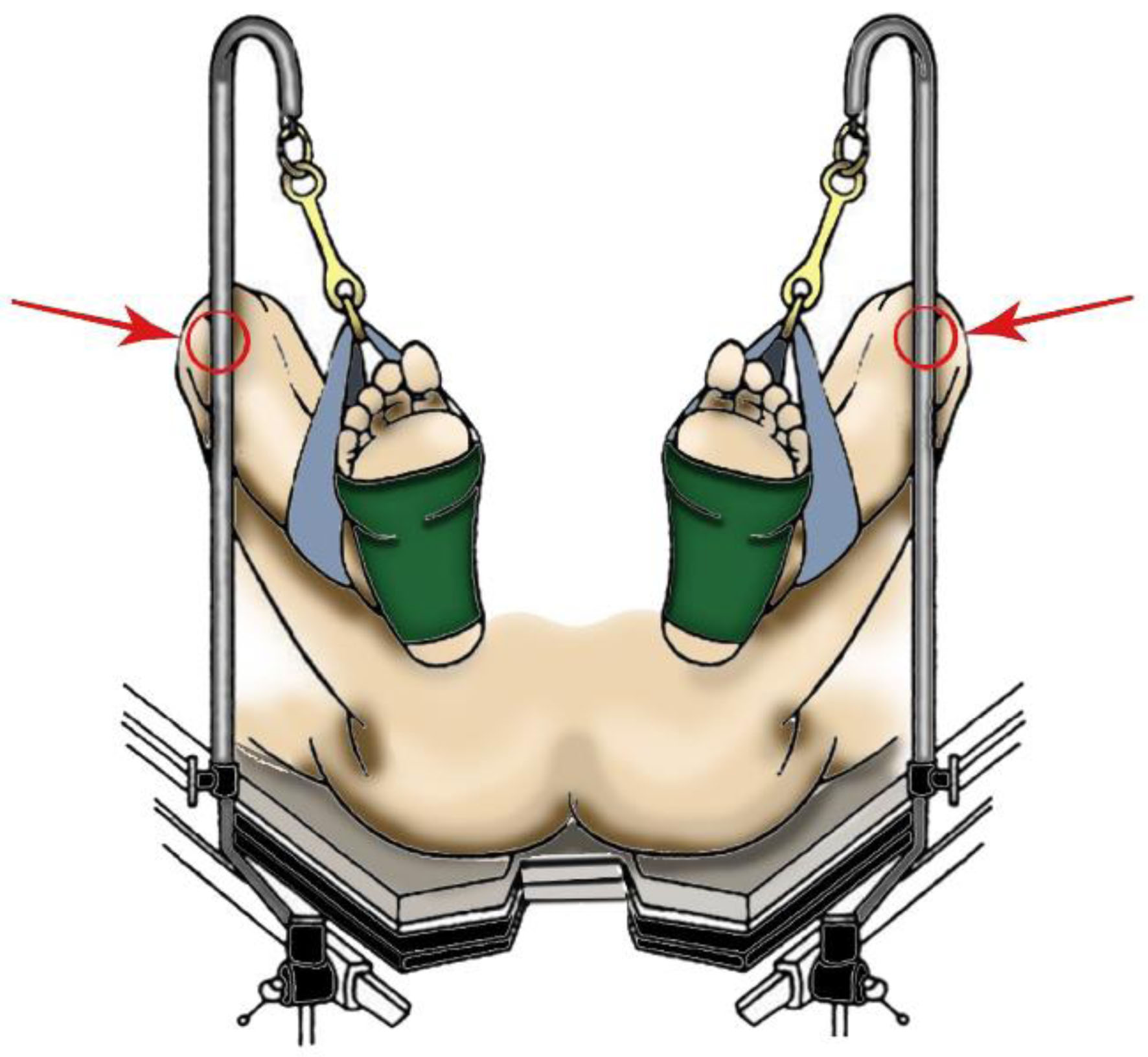 Click for large image | Figure 2. Inappropriate positioning of a patient in lithotomy position with potential to cause common peroneal nerve injury against bar holding stirrups in place (red arrow). |
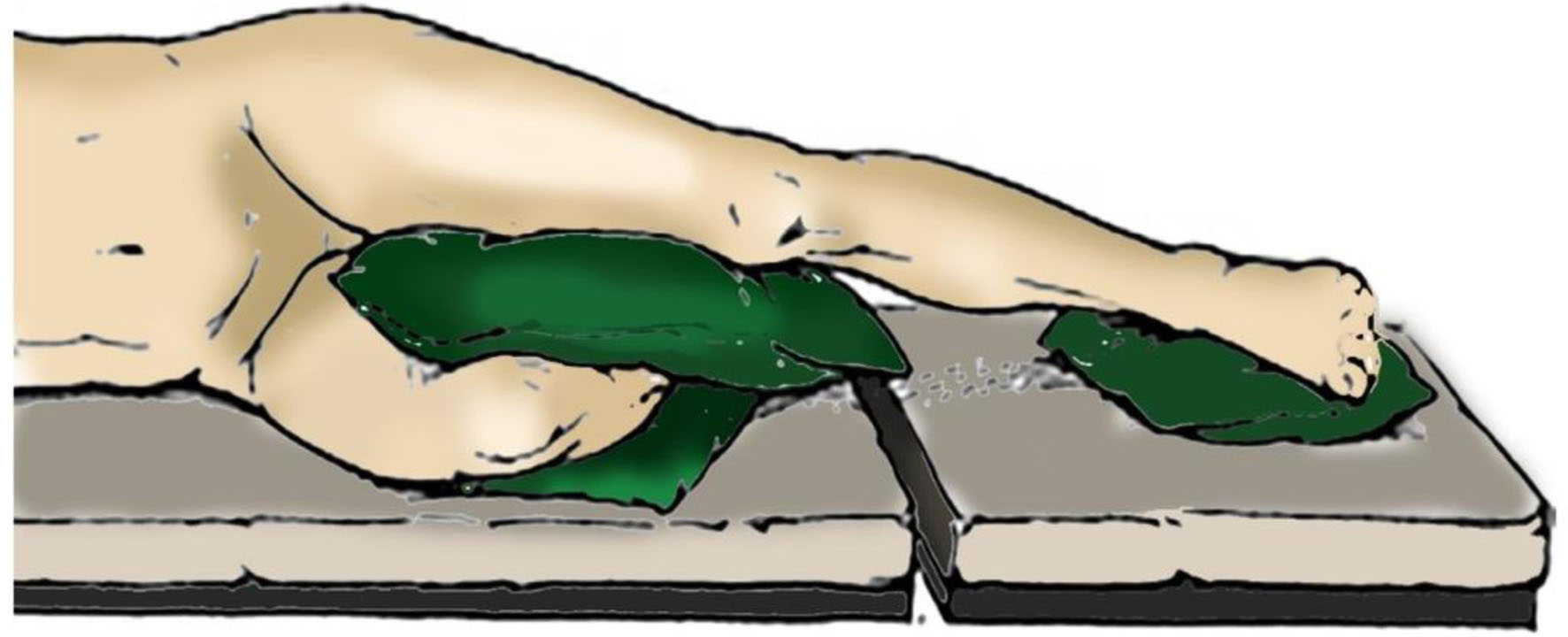 Click for large image | Figure 3. Demonstration of appropriate padding for patient in lateral decubitus position. |
 Click to view | Table 1. Reports of Foot Drop in Association With Neuraxial Anesthesia |
When a significant motor of sensory deficit is noted which is not attributable to the epidural infusion, diagnostic workup starts with an emergent evaluation for the possible treatable causes of foot drop, most importantly an epidural hematoma, as early intervention can result in improved prognosis and recovery [28, 29]. The epidural infusion should be discontinued. The evaluation generally consists of a focused history and physical examination, imaging, and neurophysiological studies. MRI is preferable for delineation of epidural and spinal cord pathology including neuraxial hematoma formation. If MRI is unremarkable, MR neurography may proceed to exclude peripheral nerve compression or common peroneal nerve injury. In our patient, MRI of the lower extremity demonstrated neuronal injury to the common peroneal nerve, likely due to perioperative compression. We postulate that the injury most likely occurred intraoperatively during the 17-h surgical procedure as access to the extremity contralateral to the surgical site was limited by the surgical drapes and patient positioning. However, postoperative compressive injury may also occur, especially in a patient with restricted postoperative mobility and sensory blockade from epidural analgesia.
Conclusion
We present a case of perioperative contralateral foot drop following lower extremity tumor resection in a patient with an epidural catheter in place. Emergent MRI was performed to exclude the possibility of neuraxial compression by hematoma or other reversible causes of foot drop. Subsequently, MR neurography of the lower extremity revealed a common peroneal nerve injury (neuropraxia) from positioning or external compression. Given the presumed mechanism of injury, recovery was expected with conservative treatment. However, immediate investigation is indicated to rule out a surgical emergency (epidural hematoma) whenever neurologic deficits are noted in patients receiving epidural analgesia.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Written consent was obtained for anesthetic care and use of de-identified patient information for publication.
Author Contributions
AE contributed to case review and preparation of manuscript. GV provided clinical care of the patient and review of the drafts including final manuscript. JDT contributed to manuscript preparation, review, and editing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Weinbroum AA. Superiority of postoperative epidural over intravenous patient-controlled analgesia in orthopedic oncologic patients. Surgery. 2005;138(5):869-876.
doi pubmed - Xuan W, Hankin J, Zhao H, Yao S, Ma D. The potential benefits of the use of regional anesthesia in cancer patients. Int J Cancer. 2015;137(12):2774-2784.
doi pubmed - Neal JM, Bernards CM, Hadzic A, Hebl JR, Hogan QH, Horlocker TT, Lee LA, et al. ASRA practice advisory on neurologic complications in regional anesthesia and pain medicine. Reg Anesth Pain Med. 2008;33(5):404-415.
doi pubmed pmc - Moraca RJ, Sheldon DG, Thirlby RC. The role of epidural anesthesia and analgesia in surgical practice. Ann Surg. 2003;238(5):663-673.
doi pubmed pmc - Meyer MJ, Krane EJ, Goldschneider KR, Klein NJ. Case report: neurological complications associated with epidural analgesia in children: a report of 4 cases of ambiguous etiologies. Anesth Analg. 2012;115(6):1365-1370.
doi pubmed - Wilkinson PA, Valentine A, Gibbs JM. Intrinsic spinal cord lesions complicating epidural anaesthesia and analgesia: report of three cases. J Neurol Neurosurg Psychiatry. 2002;72(4):537-539.
doi pubmed pmc - Gupta A, Jay MA, Williams G. Evolving pediatric epidural practice: An institution's clinical experience over 20 years-A retrospective observational cohort study. Paediatr Anaesth. 2020;30(1):25-33.
doi pubmed - Liu H, Brown M, Sun L, Patel SP, Li J, Cornett EM, Urman RD, et al. Complications and liability related to regional and neuraxial anesthesia. Best Pract Res Clin Anaesthesiol. 2019;33(4):487-497.
doi pubmed - Campos MG, Peixoto AR, Fonseca S, Santos F, Pinho C, Leite D. Assessment of main complications of regional anesthesia recorded in an acute pain unit in a tertiary care university hospital: a retrospective cohort. Braz J Anesthesiol. 2022;72(5):605-613.
doi pubmed pmc - Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104(4):965-974.
doi pubmed - Bhorkar NM, Dhansura TS, Tarawade UB, Mehta SS. Epidural hematoma: vigilance beyond guidelines. Indian J Crit Care Med. 2018;22(7):555-557.
doi pubmed pmc - Lawton MT, Porter RW, Heiserman JE, Jacobowitz R, Sonntag VK, Dickman CA. Surgical management of spinal epidural hematoma: relationship between surgical timing and neurological outcome. J Neurosurg. 1995;83(1):1-7.
doi pubmed - Han IS, Chung EY, Hahn YJ. Spinal epidural hematoma after epidural anesthesia in a patient receiving enoxaparin -A case report. Korean J Anesthesiol. 2010;59(2):119-122.
doi pubmed pmc - Poage C, Roth C, Scott B. Peroneal nerve palsy: evaluation and management. J Am Acad Orthop Surg. 2016;24(1):1-10.
doi pubmed - Morgan KJ, Figueroa JJ. An unusual postoperative neuropathy: foot drop contralateral to the lateral decubitus position. A Case Rep. 2016;7(5):115-117.
doi pubmed - Hsu KL, Chang CW, Lin CJ, Chang CH, Su WR, Chen SM. The dangers of hemilithotomy positioning on traction tables: case report of a well-leg drop foot after contralateral femoral nailing. Patient Saf Surg. 2015;9:18.
doi pubmed pmc - Lee SH, Hwang HP, Yoon SJ. Open Sciatic nerve decompression for compartment syndrome after prolonged lithotomy position: a case report. Medicina (Kaunas). 2022;58(10):1497.
doi pubmed pmc - Vladinov GM, Glick B, Aguirre HO, Fiala RS, Maga JM. Lower extremity injury while undergoing urology procedures in the Trendelenburg with lithotomy position: three case reports. J Perianesth Nurs. 2021;36(3):214-218.
doi pubmed - Kida K, Hara K, Sata T. [Postoperative palsies of the common peroneal nerve and the tibial nerve associated with lateral position]. Masui. 2013;62(2):217-219.
pubmed - Singh R, Singh P, Lhingnunmawi S. Foot drop - An unusual complication of epidural anaesthesia in a child. Indian J Anaesth. 2022;66(9):674-675.
doi pubmed pmc - Yigit NA, Bagbanci B, Celebi H. Drop foot after pediatric urological surgery under general and epidural anesthesia. Anesth Analg. 2006;103(6):1616.
doi pubmed - Nirmala B, Kumari G. Foot drop after spinal anaesthesia: A rare complication. Indian J Anaesth. 2011;55(1):78-79.
doi pubmed pmc - Ahmad FU, Pandey P, Sharma BS, Garg A. Foot drop after spinal anesthesia in a patient with a low-lying cord. Int J Obstet Anesth. 2006;15(3):233-236.
doi pubmed - Dorjey Y. Bilateral foot drop after spinal anesthesia for cesarean section. Int J Gynaecol Obstet. 2022;158(2):484-487.
doi pubmed - Kantekin CU, Beger B, Daar G. A Child Develops Drop Foot after Spinal Anaesthesia. Balkan Med J. 2015;32(3):331-332.
doi pubmed pmc - Lin Y, Chen KB, Chen LK. Prolonged postpartum foot drop after cesarean section in a patient with perineural cyst. Taiwan J Obstet Gynecol. 2021;60(5):963-964.
doi pubmed - Chen X, Xu Z, Lin R, Liu Z. Persistent cauda equina syndrome after cesarean section under combined spinal-epidural anesthesia: a case report. J Clin Anesth. 2015;27(6):520-523.
doi pubmed - Carolus AE, Becker M, Cuny J, Smektala R, Schmieder K, Brenke C. The interdisciplinary management of foot drop. Dtsch Arztebl Int. 2019;116(20):347-354.
doi pubmed pmc - Oosterbos C, Rasulic L, Rummens S, Kiekens C, van Loon J, Lemmens R, Theys T. Controversies in treatment strategies in patients with foot drop due to peroneal nerve entrapment: Results of a survey among specialists. Brain Spine. 2022;2:100887.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
