| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website http://www.theijcp.org |
Case Report
Volume 1, Number 4-5, October 2012, pages 124-128
Mumps-virus-associated Clinically Mild Encephalopathy With a Reversible Splenial Lesion
Kaori Kimuraa, Tatsuo Fuchigamia, d, Wakako Ishiia, Yuki Imaia, Satomi Tanabea, Remi Kuwabaraa, Yukihiko Fujitab, Hideo Mugishimaa, Katsuo Aokic
aDepartment of Pediatrics and Child Health, Nihon University School of Medicine, Tokyo 173-8610, Japan
bDivision of Medical Education Planning, Nihon University School of Medicine, Tokyo 173-8610, Japan
cDivision of Pediatrics, IMS Memorial Hospital, Tokyo 174-0071, Japan
dCorresponding author: Tatsuo Fuchigami, Department of Pediatrics and Child Health, Nihon University School of Medicine, 30-1 Oyaguchi-Kamicho, Itabashi-ku, Tokyo 173-8610, Japan
Manuscript accepted for publication October 3, 2012
Short title: Clinically Mild Encephalopathy
doi: https://doi.org/10.4021/ijcp51w
| Abstract | ▴Top |
Mumps virus infection primarily involves the parotid glands and most frequently affects young children during the winter and spring months. It is known that mumps virus infection may be accompanied by neurological manifestations, including meningitis and encephalitis. However, few cases of acute encephalopathy have been reported to date. We report a case of a 4-year-old girl with clinically mild encephalopathy with a reversible splenial lesion associated with mumps virus infection. She had swelling of the bilateral parotid glands. She was admitted to our hospital because of reduced level of consciousness, seizures, and vomiting. Cell counts in the cerebrospinal fluid (CSF) were normal. She had a low serum sodium level on admission. Brain computed tomography showed mild cerebral edema. Electroencephalography showed partial high-voltage slow waves at the occipital lesion, and diffusion-weighted magnetic resonance imaging demonstrated a transient abnormality in the splenium of the corpus callosum. We diagnosed clinically mild encephalopathy with a reversible splenial lesion associated with mumps virus infection. She recovered well, and exhibited no neurological sequelae. Mumps virus RNA was not detected in the CSF, suggesting that the reversible splenial change was caused by indirect effects on the central nervous system subsequent to viral infection. Her low serum sodium level also indicates that this change can occur with hyponatremia.
Keywords: Corpus callosum; Diffusion-weighted imaging; Encephalopathy; Mumps virus; Splenial lesion
| Introduction | ▴Top |
Mumps is a common childhood infection caused by the mumps virus. The hallmark of infection is swelling of the parotid gland. Aseptic meningitis and encephalitis are common complications of mumps, together with orchitis and oophoritis, which can arise in adult men and women, respectively; other complications include deafness and pancreatitis [1]. In 2004, Tada et al [2] identified clinically mild encephalitis/encephalopathy with a reversible splenial lesion (MERS) as a new type of acute encephalopathy, characterized by transient splenial lesions with high-signal intensity on diffusion-weighted magnetic resonance imaging (MRI), a mild clinical course, and a good outcome. MERS has been associated with various infectious diseases. Influenza virus A and B are the most common pathogens, following by mumps virus, adenovirus, rotavirus, streptococci, and Escherichia coli in Japan [3]. Although there are some reports of MERS associated with mumps virus infection [2, 4], these three cases were all meningoencephalitis and showed pleocytosis with a reversible splenial lesion. The mechanisms of mumps-virus-associated MERS remain unclear.
We report a patient with mumps-virus-associated encephalopathy (without pleocytosis) with a reversible splenial lesion with high-signal intensity on diffusion-weighted MRI. Serum sodium level and the result of viral RNA testing of cerebrospinal fluid (CSF) samples are discussed to elucidate the possible mechanisms of MERS.
| Case Report | ▴Top |
A previously healthy 4-year-old girl experienced fever (38.8 °C) with swelling of the left side parotid glands for 1 day before hospitalization. She visited a general hospital, and was diagnosed with mumps. The following day, she developed swelling of the bilateral parotid glands, and had headache and recurrent vomiting. She visited the previous hospital again and was admitted in the evening. She had neck stiffness. A lumbar puncture was taken, with suspected diagnosis of mumps meningitis. However, her CSF revealed no increased cell count. She had generalized tonic seizures lasting about 3 min at night. She was transferred to the Department of Pediatrics, Nihon University School of Medicine Itabashi Hospital, Tokyo, Japan. She was then admitted to our hospital on the second day from onset. Her developmental history was normal, and she had no seizures. She had no history of mumps infection and had not received mumps vaccination.
On admission, she had a temperature of 39.8 °C, heart rate of 148 beats/min, blood pressure of 101/67 mmHg, and respiratory rate of 20 breaths/min. She had delirium with a Glasgow Coma Scale score of E4 V4 M6. Neurological examination showed no abnormality except for her reduced level of consciousness. She had swelling of the bilateral parotid and submandibular glands. She had a positive Kernig’s sign as well as nuchal rigidity. Her chest and abdomen showed no abnormal findings.
Laboratory blood testing showed a leukocyte count of 5,600/µL, hemoglobin 15.0 g/dl, platelet count 131,000/µL, serum Na 131 mEq/L, K 4.5 mEq/L, Cl 93 mEq/L, blood urea nitrogen 16.1 mg/dL, creatinine 0.58 mg/dL, aspartate aminotransferase 51 U/L, alanine aminotransferase 16 U/L, lactate dehydrogenase 307 U/L, creatine kinase 91 U/L, amylase 1266 U/L, glucose 124 mg/dL, and C-reactive protein 3.14 mg/dL. The laboratory data demonstrated a decrease in the levels of serum sodium to 131 mEq/L, and increased urinary sodium of 54 mEq/L and urinary osmolality of 552 mOsm/kg, which suggested that she had inappropriate antidiuretic hormone secretion syndrome (SIADH). CSF analysis did not show any pleocytosis, elevation in protein, or reduction in glucose. The patient was determined to be positive for mumps-specific IgM antibody by enzyme-linked immunosorbent assay. Reverse transcriptase polymerase chain reaction did not reveal mumps virus in the CSF on admission. Brain computed tomography was performed on the day of admission (second day from onset), and it did not reveal any space-occupying lesion or bleeding. However, it revealed mild brain edema. Brain MRI was also performed on the second day of admission (third day from onset). T1- and T2-weighted images did not reveal any structural abnormalities. Diffusion-weighted MRI showed a focal, high-intensity lesion in the splenium of the corpus callosum. Fluid-attenuated inversion recovery imaging also showed a slightly hyperintense lesion (Fig. 1a, b). Electroencephalography (EEG) on the second day of admission demonstrated diffuse high-voltage slow waves, which were particularly marked in the occipital area during awake recording (Fig. 2). These findings strongly suggested MERS associated with mumps virus infection. The patient was treated with intravenous osmotic diuretic (D-mannitol) and isotonic fluid infusions. Her mental state started to improve soon after the initiation of treatment, and her communication returned to normal on the second day after admission. A follow-up MRI on the eighth day of admission (ninth day from onset) revealed complete resolution of the splenial lesion (Fig. 1c). EEG on the eighth day after admission (ninth day from onset) did not show slow waves or seizure waves. On the ninth day of admission (10th day from onset), she was discharged from hospital without any neurological sequelae. After discharge, she had no further seizures and development was normal.
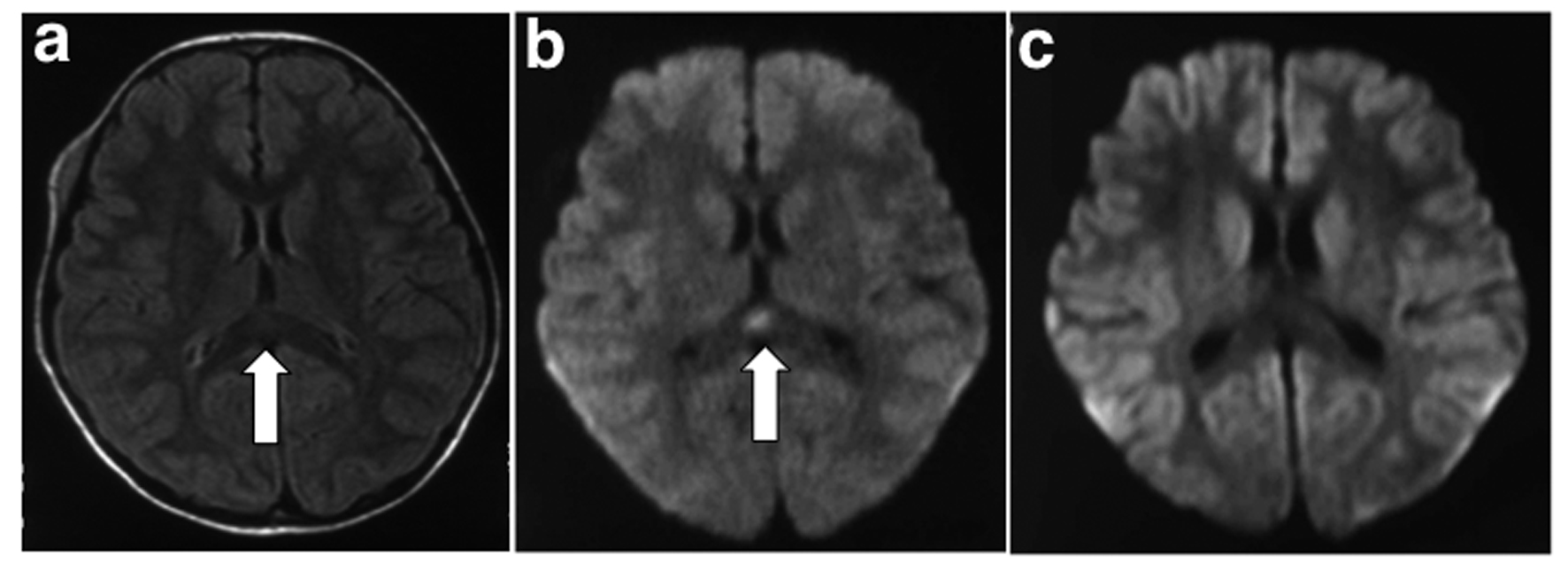 Click for large image | Figure 1. Brain magnetic resonance imaging. a: Fluid-attenuated inversion recovery image on the second day of admission (third day from onset) showed a slightly hyperintense lesion in the splenium of the corpus callosum (arrow); b: Diffusion-weighted image on the second day of admission (third day from onset) showing a focal high-intensity lesion in the splenium of the corpus callosum (arrow); c: Diffusion-weighted image on eighth day of admission (ninth day from onset) showing complete resolution of the lesion. |
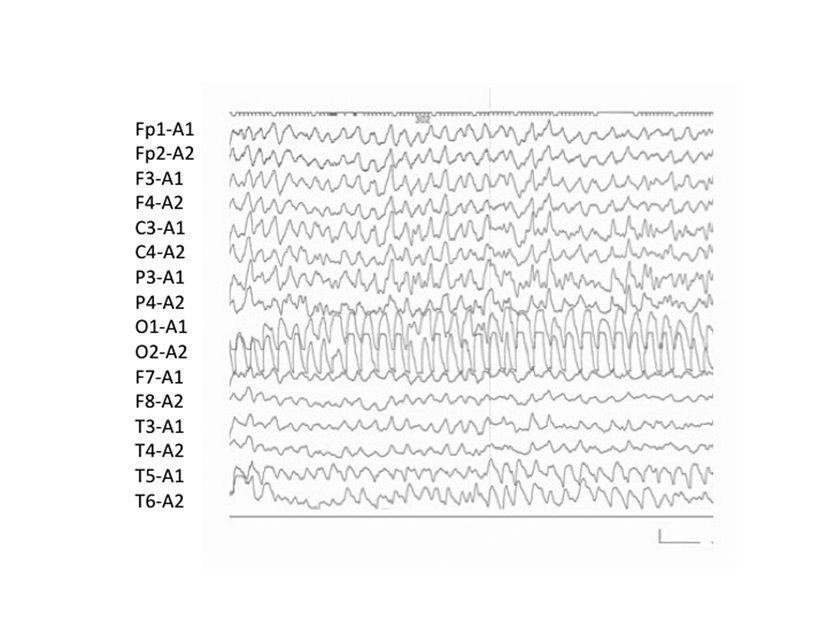 Click for large image | Figure 2. EEG in awake patient (third day from onset) showing a global diffuse, high-voltage, slow wave about 3 - 4 Hz in the particularly marked occipital area. Calibration: 100 µV, 1 s. |
| Discussion | ▴Top |
Acute encephalitis is a well-known complication of mumps virus infection; however, few cases of acute encephalopathy have been reported to date [5]. Recently, a total of 983 cases reportedly had acute encephalopathy during 2007 - 2010 in Japan [6]. Among the pathogens of the preceding infection, influenza virus was the most common (26%), followed by human herpesvirus (HHV)-6 (17%), rotavirus (4.0%), respiratory syncytial virus (1.7%), and mumps virus (0.9%). Among syndromes of acute encephalopathy, acute encephalopathy with biphasic seizures and late reduced diffusion (28.7%) was the most frequent, followed by MERS (15.6%), acute necrotizing encephalopathy (4.0%). In 153 cases with MERS, pathogens of the preceding infection were influenza virus (34.4%), rotavirus (11.7%), mumps virus (3.9%), HHV-6 (2.0%), and bacterial (3.3%) infections. These results showed that cases of mumps-virus-associated acute encephalopathy and MERS were rare [3, 5, 6]. Three pediatric patients with MERS associated with mumps virus infection have previously been reported [2, 4]. These cases were all with meningoencephalitis, and no encephalopathy. However, our case of mumps-associated MERS was with encephalopathy and revealed no increased cell count in CSF. The outcome was excellent in all cases with mumps-associated MERS, including our present case (Table 1). Hara et al have reported a case of MERS after mumps vaccination, and this case was also with encephalitis, as revealed by an increased cell count of 624/mm3 in CSF [7]. The sequence of mumps virus obtained from the patient was identical to that of the vaccine strain. This implies that the vaccine strain was strongly associated with MERS in that case. Nine patients with mumps-virus-associated encephalopathy have been reported in Japan in the past 20 years [5]. Although the prognosis in all cases with mumps-virus-associated MERS was excellent, all patients with mumps-virus-associated encephalopathy experienced progressive coma and/or seizures, and their prognoses varied from having no sequelae to death.
 Click to view | Table 1. Previously Published Reports of MERS Associated With Mumps Virus Infection |
Although several viruses have been associated with MERS, the pathophysiological mechanisms remain unclear. We previously have examined the CSF of six patients with seizures associated with rotavirus infection, and detected viral genes in all of the samples [8]. However, rotavirus antigen and RNA have not been detected in the CSF of patients with rotavirus-associated MERS, including our present case [9-12]. These findings suggest that rotavirus-associated MERS is not caused by direct invasion, but by indirect effects on the central nervous system. However, CSF testing for rotavirus antigen and RNA has not been undertaken in enough cases for this to be definitively concluded.
It has been proposed that MERS may be caused by intramyelinic axonal edema or local inflammatory cell infiltration [2]. Previous studies have reported a close relationship between MERS and hyponatremia involving SIADH. Takanashi et al [13] have reported that most patients with MERS had mild hyponatremia. Hypotonic hyponatremia results in entry of water into the brain, resulting in cerebral edema, headache, nausea, vomiting, confusion, and seizures. It is clinically difficult to separate MERS from hyponatremic encephalopathy, or to rule out hyponatremia as a contributing factor to MERS. Our patient had also a low serum sodium level (Na 131 mEq/L) on admission, and had similar symptoms, such as nausea, vomiting, confusion, and seizure. This finding also indicates that mumps-virus-associated MERS can develop with hyponatremia.
Virus-associated acute encephalopathy is believed to be related to the cytokine storm of varying degrees [14]. There have been several previous reports of elevated interleukin (IL)-6 and soluble tumor necrosis factor receptor-1 levels in the CSF in cases of acute encephalopathy associated with influenza virus [15] and mumps virus [5] infection. IL-6 and nitric oxide metabolites (nitrites and nitrates) have been suggested as potential contributing factors to MERS. IL-6 level was measured in the CSF of a previously reported case of rotavirus-associated MERS, and was found to be extremely high at 952.0 pg/mL (normal 6–71 pg/mL) [11]. Such a high level of IL-6 suggests significant inflammation of the central nervous system, which may result in an increase in vascular permeability, with or without direct virus invasion. We did not measure IL-6 and nitric oxide metabolite levels in this case.
The present case supports the theory that mumps-virus-associated MERS is not caused by direct viral invasion of the central nervous system. Our patient had a low serum sodium level, indicating that mumps-virus-associated MERS can develop with hyponatremia. IL-6 and nitric oxide metabolites may also contribute to the development of this condition. Further research is required to evaluate this possibility, and improve our understanding of the mechanisms by which mumps virus infection causes neurological sequelae, including mumps-virus-associated MERS.
Informed Consent
Informed written consent for publication of this case was obtained from the patient’s parents.
Conflict of Interest
The authors declare no potential conflicts of interests with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
| References | ▴Top |
- Hviid A, Rubin S, Muhlemann K. Mumps. Lancet. 2008;371(9616):932-944.
doi - Tada H, Takanashi J, Barkovich AJ, Oba H, Maeda M, Tsukahara H, Suzuki M, et al. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology. 2004;63(10):1854-1858.
doi pubmed - Takanashi J. Two newly proposed infectious encephalitis/encephalopathy syndromes. Brain Dev. 2009;31(7):521-528.
doi pubmed - Matsumoto N, Narahara K, Kiguchi T, Kobatake C, Yamaguchi I, Kawata J, Ando Y, et al. Reversible splenial lesion of the corpus callosum in a patient with mumps meningoencephalitis [in Jananese with English abstract]. J Jpn Pediatr Soc. 2009; 113(11): 1717-1720.
- Watanabe M, Suyama K, Hashimoto K, Sato M, Ohara S, Abe Y, Kawasaki Y, et al. Mumps Virus-Associated Acute Encephalopathy: Case Report and Review of the Literature. J Child Neurol. 2012.
doi - Hoshino A, Saitoh M, Oka A, Okumura A, Kubota M, Saito Y, Takanashi J, et al. Epidemiology of acute encephalopathy in Japan, with emphasis on the association of viruses and syndromes. Brain Dev. 2012;34(5):337-343.
doi pubmed - Hara M, Mizuochi T, Kawano G, Koike T, Shibuya I, Ohya T, Ohbu K, et al. A case of clinically mild encephalitis with a reversible splenial lesion (MERS) after mumps vaccination. Brain Dev. 2011;33(10):842-844.
doi pubmed - Liu B, Fujita Y, Arakawa C, Kohira R, Fuchigami T, Mugishima H, Kuzuya M. Detection of rotavirus RNA and antigens in serum and cerebrospinal fluid samples from diarrheic children with seizures. Jpn J Infect Dis. 2009;62(4):279-283.
pubmed - Fukuda S, Kishi K, Yasuda K, Sejima H, Yamaguchi S. Rotavirus-associated encephalopathy with a reversible splenial lesion. Pediatr Neurol. 2009;40(2):131-133.
doi pubmed - Arakawa C, Fujita Y, Imai Y, Ishii W, Kohira R, Fuchigami T, Mugishima H, et al. Detection of group a rotavirus RNA and antigens in serum and cerebrospinal fluid from two children with clinically mild encephalopathy with a reversible splenial lesion. Jpn J Infect Dis. 2011;64(3):204-207.
pubmed - Mori T, Morii M, Kuroiwa Y, Hotsubo T, Fuse S, Tsustumi H. Rotavirus encephalitis and cerebellitis with reversible magnetic resonance signal changes. Pediatr Int. 2011;53(2):252-255.
doi pubmed - Fuchigami T, Goto K, Hasegawa M, Saito K, Kida T, Hashimoto K, Fujita Y, et al. A 4-year-old girl with clinically mild encephalopathy with a reversible splenial lesion associated with rotavirus infection. J Infect Chemother. 2012.
doi - Takanashi J, Tada H, Maeda M, Suzuki M, Terada H, Barkovich AJ. Encephalopathy with a reversible splenial lesion is associated with hyponatremia. Brain Dev. 2009;31(3):217-220.
doi pubmed - Mizuguchi M, Yamanouchi H, Ichiyama T, Shiomi M. Acute encephalopathy associated with influenza and other viral infections. Acta Neurol Scand Suppl. 2007;186: 45-56.
doi - Ichiyama T, Morishima T, Isumi H, Matsufuji H, Matsubara T, Furukawa S. Analysis of cytokine levels and NF-kappaB activation in peripheral blood mononuclear cells in influenza virus-associated encephalopathy. Cytokine. 2004;27(1):31-37.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
