| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website https://www.theijcp.org |
Original Article
Volume 10, Number 4, December 2021, pages 70-74
The Role of a Disability in Children in Manifesting a Dermatological Disease
Department of Nutritional Sciences and Dietetics and ex. Department of Aesthetic and Cosmetology, International Hellenic University, Thessaloniki, Greece
Manuscript submitted November 16, 2021, accepted December 6, 2021, published online December 31, 2021
Short title: Dermatological Differences in Disability
doi: https://doi.org/10.14740/ijcp470
| Abstract | ▴Top |
Background: Sometimes there are differences in the appearance of skin diseases among patients who belong to different age or work groups. It is well known that some dermatological diseases are more common in children in comparison to other age groups. At least one out of 50 children has a kind of disability. The degree of their disability is crucial for their social life. We researched if there are differences in the manifestation of dermatological diseases between children with disabilities and children without disabilities and the role of a disability in creating a dermatological disease.
Methods: We examined 76 children with a dermatological disease. Half of them had a serious disability and the other half was the control group.
Results: The most common dermatological diseases in the control group were the transmissible infections such as warts, impetigo, etc. The transmissible dermatological diseases were almost 50% in the control group and only 10% in the group with the children with disability. The children with disability appeared more often with dermatitis and especially seborrheic dermatitis and less common with transmissible dermatological diseases.
Conclusions: The social distance between the children with disability and the other children of the same age is well known. A proof of that fact is the limited percentage of the transmissible dermatological diseases in the group of disabled children. We have noticed that seborrheic dermatitis is more often in children with mental disability who take medical treatment. Seborrheic dermatitis in children with disability without medication is as common as in the control group.
Keywords: Dermatology; Children; Disability; Family doctor; Psychiatry; Autism; Bullying; Pediatric dermatology
| Introduction | ▴Top |
The dermatological diseases are more than 2,500. Sometimes there are differences in the appearance of skin diseases among patients who belong to different age or work groups. Pruritus and skin cancer are more often in people aged over 65 years old [1]. Pediatric dermatology deals with skin conditions that might be a result of a dysfunction of an internal organ or a dermatological disease without internal organ participation [2]. The spectrum of the dermatological diseases in this age group is quite different than the other age groups [3]. The most frequent dermatological diseases in this group of age are skin infections from viruses or bacteria and several types of eczema [4].
Disability is a common situation and appears in almost 20% of the general population according to the Census Bureau Reports. The percentage of the people with disability is expected to increase [5].
One in nine children has a kind of disability and receives special education services [6]. There are different kinds of disabilities regarding the time of their appearance. Some of them manifest at the date of birth, some of them appear later and others are the result of an external injury [7].
There are many types of disability such as cerebral palsy, autism, attention deficit hyperactivity disorder, mobility disabilities, other mental disabilities, etc. [8].
The situation of each disability is different [9]. The common finding of all disabilities is the difficulty of these persons to have a normal life without social exclusions and special needs [10].
Some skin conditions occur in the context of a neurological syndrome. Trichothiodystrophy is sometimes associated to neurological conditions such as ataxia and epilepsy [11].
The size of a Port-Wine birthmark can be related with the degree of the neurological status in Sturge-Weber syndrome patients [12].
So, there are skin findings in children with intellectual disabilities and some of them are iatrogenic as medication side effect [13].
A relation between atopic dermatitis and learning disability in children has also been reported [14].
Because of the large number of children with disability, we have decided to investigate if there is a difference in the manifestation of the dermatological diseases in them compared to other children [15].
| Materials and Methods | ▴Top |
Seventy-six children were examined in our private dermatological medical office and some of the children with disability have been examined at their home between January 1, 2021 and June 30, 2021. All of the examined children were between 0 and 16 years old. The children were divided in two separate groups. One group was with the children with a kind of disability and the other one was the control group. Each group has 38 children. We excluded skin conditions related with their disability such as ichthyosis, Port-Wine hemangiomas, etc. We included skin reactions due to their medication as a side effect. The selected inclusion criteria for the control group were the age and the sex according to the age and the sex of the children with disability. We decided to include drug-induced skin reactions because they have common clinical manifestations with other skin diseases. For example, allergic dermatitis is a situation which is described not only as a medication side effect but it can also be triggered from other sources. The group of the children with a kind of disability was separated into two subgroups. One included children receiving medication for their disability and the other one included children without medication for their disability. We recorded the presence of dermatological diseases and the type of their disability, the sex and their age. The data are presented by numbers and are expressed as numbers and percentages. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
In the control group, there were 20 male and 18 female patients. The mean age was 8.1 years. The most common dermatological diseases in this group were different types of infected transmissible diseases (45%), dermatitis (15%), and acne (15%). Other dermatological diseases that they have manifested were urticaria, hemangiomas, vitiligo and onychodystrophy.
The transmissible dermatological diseases included impetigo (20%), warts (15%) and molluscum contagiosum (10%) (Fig. 1, Table 1).
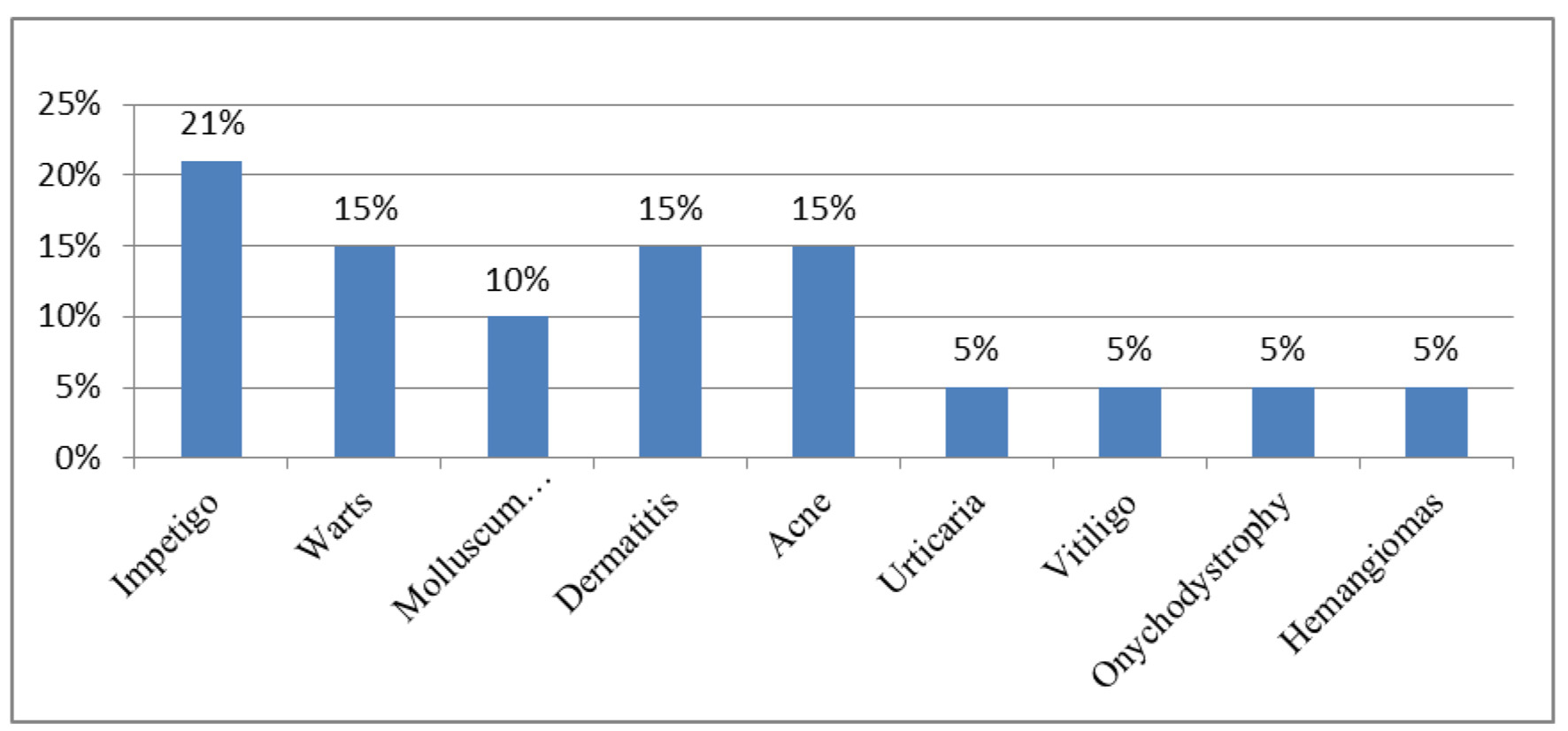 Click for large image | Figure 1. Dermatological diseases in control group. |
 Click to view | Table 1. Dermatological Diseases in the Control Group |
In the group with the children with a disability, there were 20 male and 18 female patients. The mean age was 12.05 years.
The spectrum of the disabilities included cerebral palsy, mental disabilities (e.g., autism and attention deficit hyperactivity disorder), Down syndrome and movement disabilities. One of the most common mental disabilities was autism (21%) (Table 2).
 Click to view | Table 2. Children With Disability |
The most common dermatological diseases in this group were seborrheic dermatitis (35%), atopic dermatitis (20%), contact dermatitis (15%), acne (10%), warts (10%), hair loss (5%) and urticaria (5%) (Fig. 2) (Table 3).
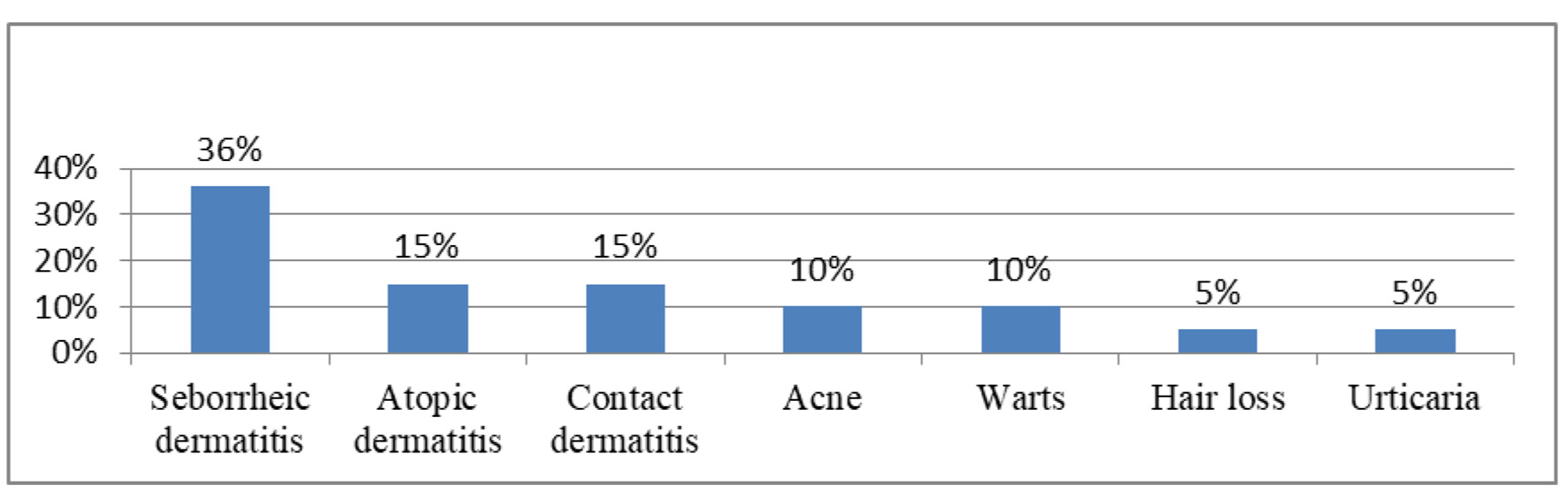 Click for large image | Figure 2. Dermatological diseases in children with disability. |
 Click to view | Table 3. Dermatological Diseases in Children With Disability |
Five out of 26 children with mental disability were under medication for their condition and they were about 19%. Seborrheic dermatitis was the most common dermatological side effect in the children with mental disability who received medication.
| Discussion | ▴Top |
Childhood skin characteristics are different from the other age groups [16]. Only 30% of the pediatric patients with a skin disorder visit a dermatologist or a pediatrician [17]. Probably some dermatological diseases such as acne present in a larger number in the community of the children than the children who finally visit a doctor. We have observed that the average age was different in the two groups. This is probably due to a delay in visiting a primary care service of the children with disability because of their condition [18]. Generally infectious diseases and different types of eczema are the most common dermatological diseases in children [19]. In our study, we have found that the most common dermatological disease in children was the transmissible infection diseases (45%) and different types of eczema (15%). In the other group, the most common dermatological diseases in children with several disabilities were seborrheic and atopic dermatitis (55%). The transmissible dermatological diseases in the second group were only 10% (Fig. 3).
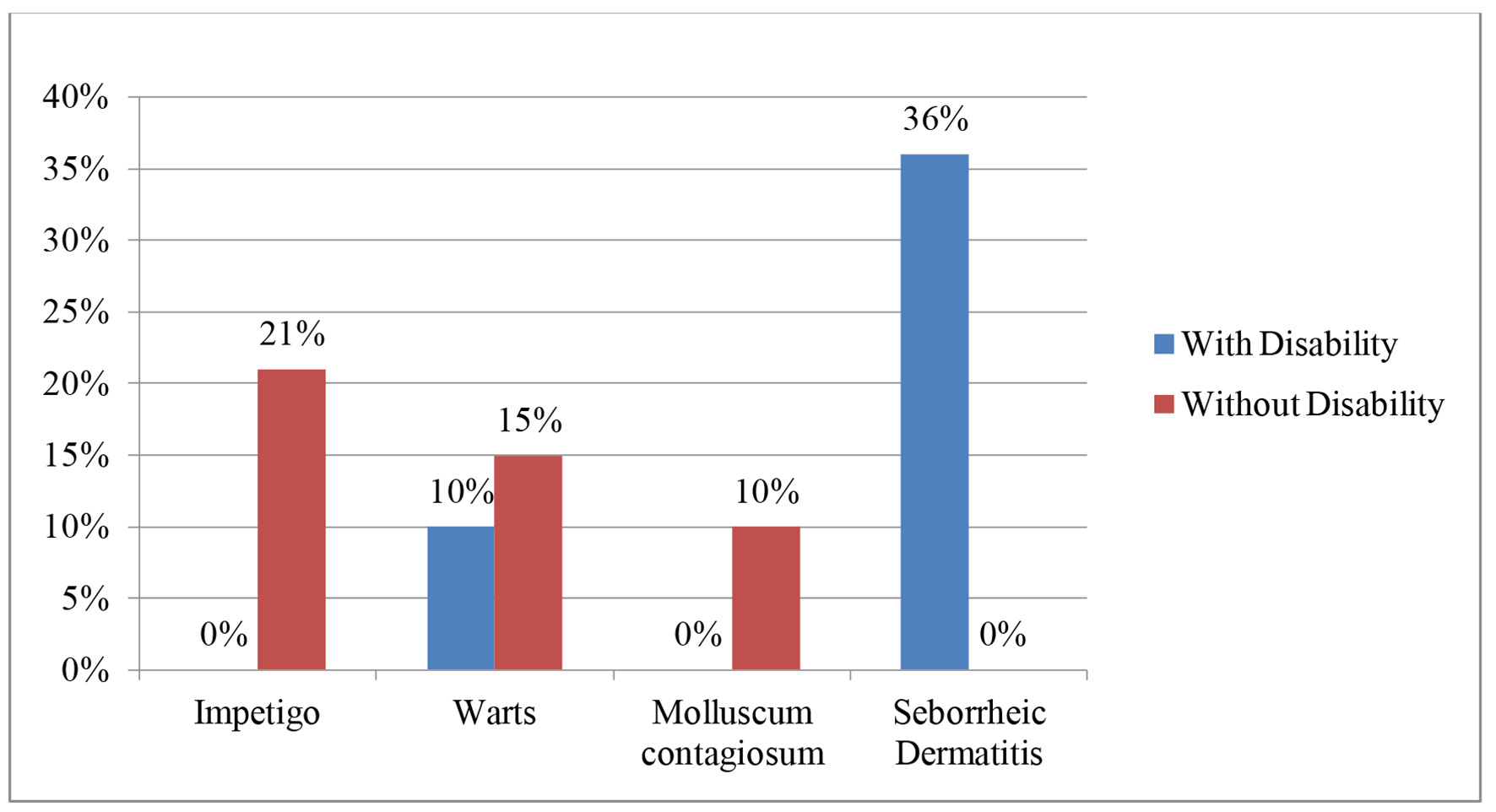 Click for large image | Figure 3. Dermatological diseases in both groups. |
The infectious dermatological disease and different kinds of eczema were the majority in both groups but their percentage was not the same. Infectious dermatological diseases manifest with higher percentage in the control group.
The children with any kind of disability are usually lonely because of the social distance. Playing with other children is not usual [20]. It is well known that social exclusion and bullying are common situations in children with disabilities [21]. Physical contact during playing is the most common reason for the transmissible dermatological diseases in children. The fact that children with special needs lack physical contact is one of the reasons that they do not often manifest transmissible dermatological diseases. Another reason is that the parents or the caregivers of these children take a great attention of their hygiene.
In contrast to the control group, the children with disability develop seborrheic dermatitis as the most common dermatological disease. Seborrheic dermatitis is a very common inflammatory chronic disease [22]. The disease appears usually in the face, the scalp, the chest with scaling, erythema and itch [23]. The disease is affected by psychological factors [24]. Seborrheic dermatitis is more common in patients who receive psychotropic drugs like haloperidol, lithium, buspirone and chloropromazine [25].
We have noticed that 19% of the children with disability have taken a kind of medication for their condition. Chronic treatment with neuroleptic induced in the most cases seborrheic dermatitis [26].
The decreased social participation creates psychological disorders in people with disabilities and their families [27]. Although children with disabilities are supported by special education programs, their integration into society continues to present difficulties.
In cases of chronic neuroleptic treatment, there should be the cooperation of a psychiatrist and a dermatologist or a general practitioner in order to reduce as much as possible the side effects on the skin [28]. Since dermatological diseases are usually visible in those cases, they might aggravate the social distance. The family and the special trainers play an active role in the reduced presence of dermatological infections by following the rules of hygiene [29].
Conclusion
Children with disabilities differ from other children of their age not only because of the cause of their disability. The finding from this study is that these children suffer less from transmissible dermatological diseases compared to other children. Unfortunately, a possible cause for this finding is probably the social exclusion.
Different types of dermatitis were identified in both groups. Seborrheic dermatitis and atopic dermatitis were clearly more common in children with disability. This finding is expected in children who either take psychotropic drugs or belong to psychiatric categories of disability such as autism.
Acknowledgments
None to declare.
Financial Disclosure
There was no specific funding source to be mentioned.
Conflict of Interest
The author declares no conflict of interest.
Informed Consent
The patients’ parents were informed about the data collection and gave their written consent.
Data Availability
The author declares that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Papadopoulos I. Comparative study of dermatological diseases of the elderly in relation to the rest population. Clin Cosmet Investig Dermatol. 2020;13:173-178.
doi pubmed - Hayden GF. Skin diseases encountered in a pediatric clinic. A one-year prospective study. Am J Dis Child. 1985;139(1):36-38.
doi pubmed - Khalifa KA, Al-Hadithi TS, Al-Lami FH, Al-Diwan JK. Prevalence of skin disorders among primary-school children in Baghdad governorate, Iraq. East Mediterr Health J. 2010;16(2):209-213.
doi pubmed - Ozcelik S, Kulac I, Yazici M, Ocal E. Distribution of childhood skin diseases according to age and gender, a single institution experience. Turk Pediatri Ars. 2018;53(2):105-112.
doi pubmed - Bickenbach JE, Cieza A, Sabariego C. Disability and public health. Int J Environ Res Public Health. 2016;13(1):123.
doi - Whitbread KM. The physician's role in educational planning for students with developmental disabilities. Conn Med. 2004;68(8):515-518.
- Johnson CP, Myers SM, American Academy of Pediatrics Council on Children With Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183-1215.
doi pubmed - Bindawas SM, Vennu V. The national and regional prevalence rates of disability, type, of disability and severity in Saudi Arabia - Analysis of 2016 demographic survey data. Int J Environ Res Public Health. 2018;15(3):419.
doi pubmed - Madans JH, Mont D, Loeb M. Comments on Sabariego et al. Measuring disability: comparing the impact of two data collection approaches on disability rates. Int. J. Environ. Res. Public Health, 2015, 12, 10329-10351. Int J Environ Res Public Health. 2015;13(1):ijerph13010065.
doi pubmed - Fathy H, El-Mongy S, Baker NI, Abdel-Azim Z, El-Gilany A. Prevalence of skin diseases among students with disabilities in Mansoura, Egypt. East Mediterr Health J. 2004;10(3):416-424.
doi pubmed - Bracun R, Hemmer W, Wolf-Abdolvahab S, Focke M, Botzi C, Killian W, Gotz M, et al. Diagnosis of trichothiodystrophy in 2 siblings. Dermatology. 1997;194(1):74-76.
doi pubmed - Dymerska M, Kirkorian AY, Offermann EA, Lin DD, Comi AM, Cohen BA. Size of facial port-wine birthmark may predict neurologic outcome in Sturge-Weber syndrome. J Pediatr. 2017;188:205-209.e201.
doi pubmed - Schepis C. Cutaneous findings in children with intellectual disabilities. J Dermatol. 2013;40(1):21-26.
doi pubmed - Wan J, Shin DB, Gelfand JM. Association between atopic dermatitis and learning disability in children. J Allergy Clin Immunol Pract. 2020;8(8):2808-2810.
doi pubmed - Wenk C, Itin PH. Epidemiology of pediatric dermatology and allergology in the region of Aargau, Switzerland. Pediatr Dermatol. 2003;20(6):482-487.
doi pubmed - Schneider AM, Nelson AM. Skin microbiota: Friend or foe in pediatric skin health and skin disease. Pediatr Dermatol. 2019;36(6):815-822.
doi pubmed - Prindaville B, Antaya RJ, Siegfried EC. Pediatric dermatology: past, present, and future. Pediatr Dermatol. 2015;32(1):1-12.
doi pubmed - Morrison EH, George V, Mosqueda L. Primary care for adults with physical disabilities: perceptions from consumer and provider focus groups. Fam Med. 2008;40(9):645-651.
- Heine G, Schnuch A, Uter W, Worm M. Frequency of contact allergy in German children and adolescents patch tested between 1995 and 2002: results from the Information Network of Departments of Dermatology and the German Contact Dermatitis Research Group. Contact Dermatitis. 2004;51(3):111-117.
doi pubmed - Nowicki EA, Brown JD, Dare L. Educators' evaluations of children's ideas on the social exclusion of classmates with intellectual and learning disabilities. J Appl Res Intellect Disabil. 2018;31(1):e154-e163.
doi pubmed - Lindsay S, McPherson AC. Experiences of social exclusion and bullying at school among children and youth with cerebral palsy. Disabil Rehabil. 2012;34(2):101-109.
doi pubmed - Mameri ACA, Carneiro S, Mameri LMA, Telles da Cunha JM, Ramos ESM. History of seborrheic dermatitis: conceptual and clinico-pathologic evolution. Skinmed. 2017;15(3):187-194.
- Clark GW, Pope SM, Jaboori KA. Diagnosis and treatment of seborrheic dermatitis. Am Fam Physician. 2015;91(3):185-190.
- Situm M, Kolic M, Buljan M. [Psychodermatology]. Acta Med Croatica. 2016;70(Suppl 1):35-38.
- Berk T, Scheinfeld N. Seborrheic dermatitis. P T. 2010;35(6):348-352.
- Binder RL, Jonelis FJ. Seborrheic dermatitis: a newly reported side effect of neuroleptics. J Clin Psychiatry. 1984;45(3):125-126.
- Park S, Lee Y, Kim CE. Korean adults' beliefs about and social distance toward attention-deficit hyperactivity disorder, Tourette syndrome, and autism spectrum disorder. Psychiatry Res. 2018;269:633-639.
doi pubmed - McColl MA, Forster D, Shortt SE, Hunter D, Dorland J, Godwin M, Rosser W. Physician experiences providing primary care to people with disabilities. Healthc Policy. 2008;4(1):e129-147.
doi - Theis KA, Steinweg A, Helmick CG, Courtney-Long E, Bolen JA, Lee R. Which one? What kind? How many? Types, causes, and prevalence of disability among U.S. adults. Disabil Health J. 2019;12(3):411-421.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
