| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website https://www.theijcp.org |
Case Report
Volume 11, Number 1, March 2022, pages 14-19
Recurrent Bilateral Pleural and Pericardial Effusions due to Tuberculosis in a Child With Doose Syndrome: A Case Report
Carla Melisa Leon-Viverosa, f, Julio Cesar Ramirez-Reyesb, Daniel Juarez-Rebollarc, Luis Xochihua-Diazd, Eduardo Baltazar Barragan-Padillae
aPediatrics Department, “Lic. Adolfo Lopez Mateos” Regional Hospital of the Security and Social Institute of the State Workers, Mexico City, Mexico
bNeurology Pediatrics Department, “Lic. Adolfo Lopez Mateos” Regional Hospital of the Security and Social Institute of the State Workers, Mexico City, Mexico
cNeurosurgery Department, “Lic. Adolfo Lopez Mateos” Regional Hospital of the Security and Social Institute of the State Workers, Mexico City, Mexico
dInfectious Pediatrics Department, “Lic. Adolfo Lopez Mateos” Regional Hospital of the Security and Social Institute of the State Workers, Mexico City, Mexico
eGeneral Pediatrics Department, “Lic. Adolfo Lopez Mateos” Regional Hospital of the Security and Social Institute of the State Workers, Mexico City, Mexico
fCorresponding Author: Carla Melisa Leon-Viveros, Pediatrics Department, “Lic. Adolfo Lopez Mateos” Regional Hospital of the Security and Social Institute of the State Workers, Mexico City, Mexico
Manuscript submitted September 2, 2021, accepted December 31, 2021, published online March 7, 2022
Short title: Tuberculosis in a Child With Doose Syndrome
doi: https://doi.org/10.14740/ijcp456
| Abstract | ▴Top |
Tuberculosis (TB) is one of the 10 causes of death worldwide. According to the World Health Organization (WHO) in the 2020 Global Tuberculosis Report, 12% of all infected people correspond to children. Other reports have been published with collected data regarding extra pulmonary TB showing that it reaches 16% of incident cases in United States of America. Pleural TB is common among adolescents and is less frequent in children. Pericardial effusion due to TB is a rare manifestation of extra pulmonary TB, and the diagnosis can be hard to reach. In this paper, we describe the manifestations, diagnosis and management of children with extra pulmonary disease, specifically the simultaneous presence of two sites of TB and the approach in children with Doose syndrome. A 9-year-old male patient with an extensive medical record was admitted with unspecific lower respiratory infection symptoms. The diagnosis was reached with the GeneXpert test after 1 month of evaluation and readmission for massive pleural effusion. He required tube drainage twice and specific management with rifampicin, isoniazid, pyrazinamide and ethambutol. In this case, the symptoms were nonspecific which delayed the diagnosis. The purpose of this case is to emphasize the importance of suspicion and early diagnosis of extra pulmonary TB known as the “great mimicker”.
Keywords: Tuberculous pleural effusion; Extra pulmonary tuberculosis; Doose syndrome; Bilateral pleural effusion; Pericardial effusion
| Introduction | ▴Top |
Mycobacterium tuberculosis is a pathogen responsible for the infectious disease named tuberculosis (TB). In Mexico and other countries, it is called “the great mimicker”, because it manifests in various features, clinical and imaging depending on the affected organ.
One of the 10 causes of death worldwide is TB. Globally in 2019, it has been estimated that 10 million people were infected with TB [1].
According to the World Health Organization (WHO), in the 2020 Global Tuberculosis Report, 12% of all infected people correspond to children, affecting both sexes. The mortality rate was estimated at 17% in children between the ages of 0 and 14 years [1].
Extra pulmonary TB reaches 16% of incident cases in United States of America, less than 24% in the Eastern Mediterranean Region [1]. In children, up to 25% present as extrapulmonary [2].
TB infection commonly affects the respiratory system but it can also affect other sites. In pediatric population, the most common site is lungs, followed by lymph nodes, pleura, miliary dissemination, musculoskeletal system, meninges, pericardial space, and cutaneous, abdominal, and genitourinary system [3, 4].
Pleural TB is common among adolescents and is less frequent in children under 5 years. Although TB effusion is one of the most common manifestations, the incidence in non-endemic regions is around 3-5%, while in endemic regions, the incidence reaches 30% [1, 5-7].
Pericardial effusion due to TB is a rare manifestation of extra pulmonary TB, and the diagnosis can be hard to reach [2, 8, 9]. In this paper, we describe the manifestations, diagnosis and management of children with extra pulmonary disease, specifically the simultaneous presence of two sites of TB and the approach in children with Doose syndrome.
| Case Report | ▴Top |
A 9-year-old male patient was admitted to the emergency room with elevated temperature of 37.8 °C, blood pressure of 94/61 mm Hg, heart rate of 112 bpm, respiratory rate of 36 rpm, SatO2% of 66%, weight of 20 kg, and height of 125 cm. Important findings during physical examination showed he was hypoactive and with thoracoabdominal dissociation requiring supplemental oxygen by facemask at 10 L/min, with partial recovery. At interrogation, an increased number of seizure episodes were reported, even at night during sleep, and he had an established treatment with erythromycin (40 mg/kg/day) for 7 days by another institution.
Due to global pandemic situation and current symptoms, a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antigen test was done getting a negative result. After 1 week of evolution and persistence of symptoms, he developed tachypnea. Labs were taken, and findings without relevance were identified and reported in Table 1.
 Click to view | Table 1. Serum Analysis of Important Normochromic Normocytic Anemia |
Medical background included mother with a history of two abortions and prenatal infections during the second trimester. He was delivered vaginally at gestational age of 39.5 weeks, with weight of 2,982 g, length of 50 cm, and APGAR score of 8/9.
Milestone development showed social smile at 2 months, and head and gaze control at 3 months. Motor developments showed sitting without support at 7 months, crawling at 12 months, standing alone at 12 months, and walking alone at 24 months. Language development showed babbling at 4 months, one-word stage at 12 months, and two-word stage at 18 months. Language impairment was diagnosed at the age of 3 years.
In our patient’s case, there was a history of congenital disabilities: microtia and left unilateral atresia, bilateral syndactyly of the third, fourth, fifth finger, second and third toes, requiring six surgical procedures.
More medical background included cryptorchidism at the age of 3, which was resolved with surgery, and gastroesophageal reflux disease as a newborn, requiring pharmacological treatment with proton pump inhibitors.
At the age of 5 years, the diagnosis of myoclonic atonic epilepsy was reached after a magnetic resonance imaging (MRI) scan showed cortical dysplasia of the left frontotemporal lobe. In December 2017, he presented viral encephalitis with bilateral epileptic focus. It was not until 2019 that Doose syndrome was integrated, establishing the current treatment with valproic acid, clobazam and levetiracetam.
Previous hospitalizations included newborn jaundice with phototherapy management for 24 h, pneumonia in August 2015, and bilateral maxillary sinusitis in December 2017, ending with an epileptic episode in January 2020. The mother denied any accidents and injuries.
The patient resides with his mother in an apartment in Mexico City, and the father is not involved. He has no contact with animals and there is not exposure to fumes. He lives under unsuitable conditions, considered as social economic low incomes due to mother’s background of interrupted high school education and stayed at home mother.
Evolution
During admission in the emergency room on January 28, 2021, the approach and management consisted of a chest X-ray showing massive left pleural effusion, middle right pleural effusion, and pericardial effusion.
Clinical systemic evaluation was done without findings relevant for the actual emergency status. During physical examination, the neurological exam showed average head size with dental dysplasia, no neurocutaneous markers were seen, and no autistic activities were observed. Cranial nerve examination showed hearing loss secondary to left atresia. Motor exam showed limited function secondary to hand surgery, fast jerky movements involving both the upper and lower limbs, and unremarkable sensory and cerebellar assessment.
His hospital stay lasted 18 days without recurrent seizures under a triple anticonvulsive and a dose of immunoglobulin (1.2 g/kg) therapy with no signs of side effects. Chest X-ray and computed tomography (CT) scan showed bilateral pleural effusion, pericardiac effusion and cardiomegaly with 1.6 indexes (Figs. 1, 2).
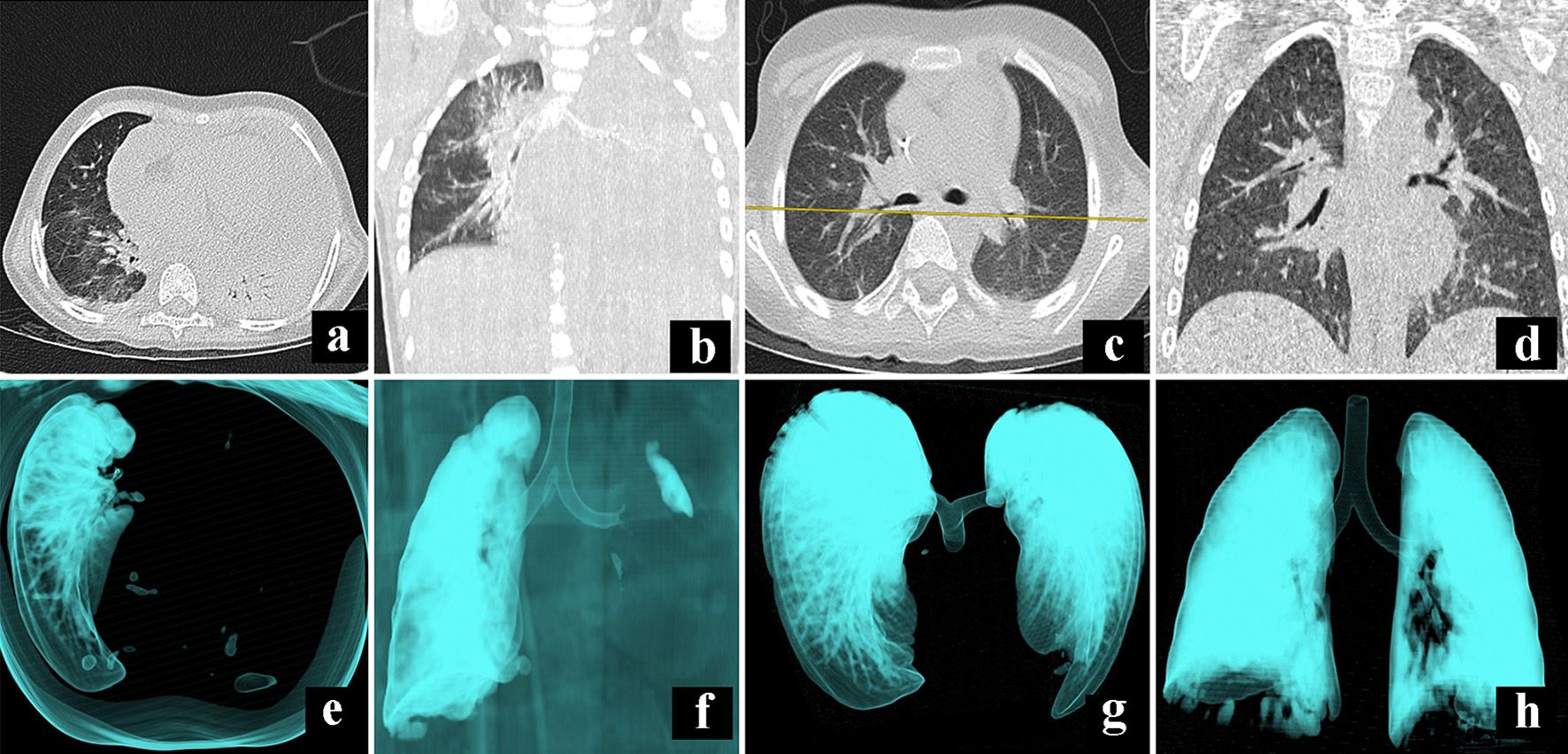 Click for large image | Figure 1. Comparative illustration of CT scan during admission (a, b, e, f) and first discharge (c, d, g, h). Panels (a) and (b) show a massive pleural effusion of the left lung that compromises all the segments; panels (e) and (f) show a 3D reconstruction to denote the occlusion of the left airway. Panels (c) and (d) show the absence of fluid in the pleural space after 18 days of treatment, while panels (g) and (h) show a full expansion of the lungs. CT: computed tomography. |
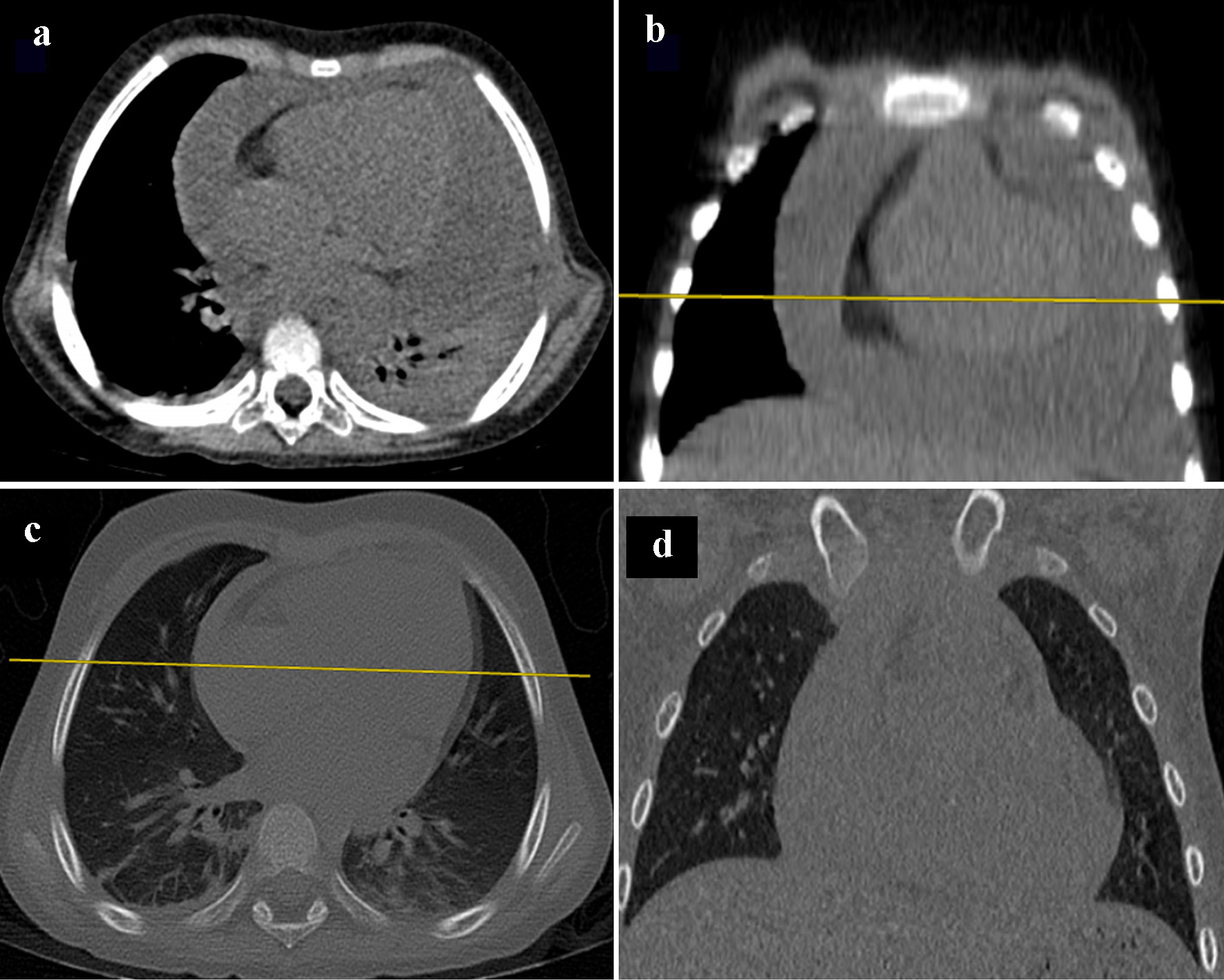 Click for large image | Figure 2. Pleural effusion image. In panels (a) and (b), CT scan of the mediastinum, with axial and coronal planes, show an increase of fluid in pericardial space. However, after treatment with diuretic therapy, comparative panels (c) and (d), the fluid collected in pleural space has diminished. CT: computed tomography. |
He required treatment with a left thoracentesis and placement of a chest tube, obtaining 20 cc of pleural fluid with the posterior analysis (Table 2). After 48 h, the collector system had drained 120 cc. He received empiric treatment with antibiotics (cefepime 100 mg/kg/day), antipyretic and analgesics for 6 days. After a follow-up chest CT showed no evidence of fluid in the pleural space and evaluation from the surgical department, the chest tube was removed. He was discharged on February 15, 2021 after a favorable evolution.
 Click to view | Table 2. Pleural Fluid Characteristics |
A week later on February 24, he was readmitted to the emergency room with an acute abdominal pain, which increased during a period of 24 h, accompanied by seven episodes of loose stools, without the presence of blood or mucus, a rise in temperature (37.2 °C) and drop in pulse oximetry (87%), and no nausea or emesis. He was treated at home with nonsteroidal anti-inflammatory drugs (NSAIDs) and supplemental oxygen at 0.5 L/min with partial recovery. As part of the examination, chest X-ray and abdominal series showed massive left pleural effusion and coprostasis treated with suppository, relieving abdominal pain, supplemental oxygen with nasal prongs, reaching pulse oximetry of 95%, and drainage of the pleural cavity with thoracentesis and chest tube.
On March 3, after a month of the first acute event, a GeneXpert MTB test gave a positive result, after evaluation and follow-up with the infectology and preventive medicine department, rifampicin, isoniazid (150 mg/day), pyrazinamide and ethambutol (doTBal®) therapy was started under the TAES (strictly supervised shortened treatment) regimen. Following a serial echocardiogram and the cardiology department recommendations, the pericardic effusion was treated with diuretics without complication. After a month of hospitalization and favorable evolution, he remained afebrile, stable and the last echocardiogram showed no evidence of effusion (Fig. 3). He was discharged on March 5.
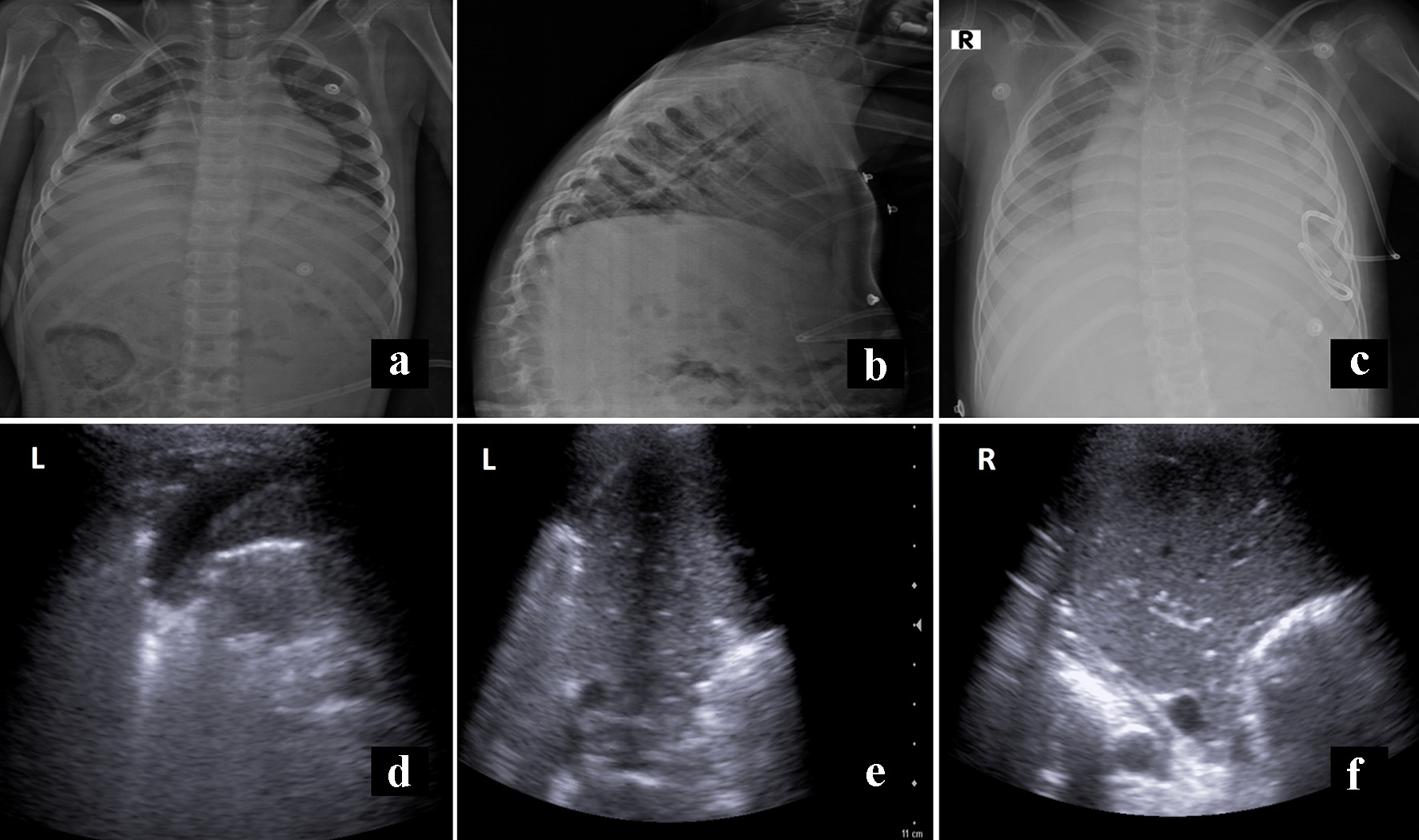 Click for large image | Figure 3. Panels (a) and (b) show the X-ray film before the first discharge without evidence of effusion. Panel (c) shows the initial film to second hospital readmission, with recurrent pleural effusion. Panels (d) and (e) correspond to sonography, previous to definitive discharge, with minimal fluid on the left side (L). In contrast, panel f shows lung parenchyma without fluid (R). |
The last evaluation was in September, and the evolution was satisfactory, without complications.
| Discussion | ▴Top |
In pleural effusion pathophysiology, the main factor is the rupture of a subpleural caseous focus, allowing antigen entry into the space. It causes an inflammatory reaction, with a subsequent increase in permeability and influx of proteins, stimulating pleural fluid formation. In addition, the occlusion of the lymphatic system in the pleura reduces the rate of clearance of fluid [5].
The diagnosis of pleural effusion due to Mycobacterium tuberculosis becomes a challenge for the pediatrician. Generally the staining and culture result negative. The reason is low bacilli in the fluid, therefore the Xpert MTB/RIF test is recommended for the analysis of pleural effusion [6, 10].
Cruz et al reported in their study of 45 patients, microbiologic findings in which only 50% were positive for the culture, and they required 60% of PCR-pleural fluid. The same percentage presents asymptomatic. In their study, 37 children required hospitalization for pleural effusion, the main reason being the need for surgical procedures (thoracentesis, pericardicentesis). Only three cases presented bilateral pleural effusion and a long hospitalization period as our case [11].
Pericardial effusion is a rare manifestation of extra pulmonary TB, but in some developing countries, there are reported cases. For example, Igoche et al reported their experience in Nigeria in 2 years with 15 children diagnosed with pericardial effusion. The most severe complication of this clinical presentation is the cardiac tamponade, for that it is challenging to suspect of this alteration [8].
In our case, the simultaneous presence of several sites of extra pulmonary TB is an uncommon finding in the pediatric population. There are few case studies of pleural and pericardial effusion in children under the age of 15 years [8, 9, 12]. Furthermore, symptoms are often nonspecific and can delay the early diagnosis.
According to Valdes et al from a large study including 254 patients, only 1.6% developed bilateral effusion. The percentage of massive pleural effusion was 18.2% [10]; this information gives more value to communicate our rare case.
Several differences were noted between this case report and other reported data in terms of age distribution and radiographic findings. For example, pleural effusion due to TB has been reported in pediatric series with 22%, and more frequently reported in adolescents [1, 2]. But our case presents prepuberal according to Cruz series [11].
In this case report, the culture yield of pleural fluid and pleural biopsy were not significantly required. Still, other studies have found that the latter is more sensitive in culture and histopathology [13].
The risk of TB infection is higher in young children, children who have been exposed recently, and children who have malnutrition, immunodeficiency (neurological conditions as epilepsy), or poor general health.
According to the International League Against Epilepsy, the last report classified epilepsy with myoclonic-atonic seizures, previously known as epilepsy with myoclonic-astatic seizures or named Doose syndrome (by Dr. Hermann Doose, 40 years ago, the first who described the features of this type of epilepsy [14]), as a syndrome characterized by seizures between 6 months and 6 years of age. In many cases, febrile convulsions and generalized tonic-clonic seizures precede the onset of myoclonic-atonic and atonic seizures [15].
Doose syndrome is relatively common with about 1 in 10,000 children (2% of childhood epilepsies), predominating in males (2:1). Neurological examination and head size are normal, and the electroencephalogram (EEG) findings are rhythmic slow-wave patterns (polyspike and wave epileptiform activity) but initially it can be normal [14-17].
Learning points
To our knowledge, there have been limited reported cases amongst the pediatric population with pleural and pericardial effusion; the underlying disease of Doose syndrome represents a challenge for the approach and the early diagnosis. This case shows the vulnerability of the pediatric population with TB disease. The purpose of this case is to emphasize the importance of an early diagnosis and suspicion of extra pulmonary TB known as a “great mimicker”.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent has been obtained.
Author Contributions
CML, JCR, and DJ drafted the initial manuscript. LX and EBB reviewed the manuscript. All the authors have approved the final manuscript as submitted and accepted accountability for all aspects of the work.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Global tuberculosis report 2020. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO. ISBN 978-92-001313-1.
- Obihara NJ, Walters E, Lawrenson J, Garcia-Prats AJ, Hesseling AC, Schaaf HS. Tuberculous pericardial effusions in children. J Pediatric Infect Dis Soc. 2018;7(4):346-349.
doi pubmed - Gopalaswamy R, Dusthackeer VNA, Kannayan S, Subbian S. Extrapulmonary. Tuberculosis-an update on the diagnosis, treatment and drug resistance. J Respir. 2021;1:141-164.
doi - Kritsaneepaiboon S, Andres MM, Tatco VR, Lim CCQ, Concepcion NDP. Extrapulmonary involvement in pediatric tuberculosis. Pediatr Radiol. 2017;47(10):1249-1259.
doi pubmed - Shaw JA, Diacon AH, Koegelenberg CFN. Tuberculous pleural effusion. Respirology. 2019;24(10):962-971.
doi pubmed - Bayhan GI, Sayir F, Tanir G, Tuncer O. Pediatric pleural tuberculosis. Int J Mycobacteriol. 2018;7(3):261-264.
doi pubmed - Lewinsohn DM, Leonard MK, LoBue PA, Cohn DL, Daley CL, Desmond E, Keane J, et al. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention Clinical Practice Guidelines: diagnosis of tuberculosis in adults and children. Clin Infect Dis. 2017;64(2):111-115.
doi pubmed - Igoche, Mustafa A, Ibrahim A. Pericardial effusion and outcome in children at a Tertiary Hospital in North-Western Nigeria: A 2-year retrospective review. Res Cardiovasc Med. 2019;8:14-18.
- Chiu NC, Wu SJ, Chen MR, Peng CC, Chang L, Chi H, Lin CY. A mysterious effusion: tuberculous pericarditis. J Pediatr. 2016;174:271-271.e271.
doi pubmed - Valdes L, Alvarez D, San Jose E, Penela P, Valle JM, Garcia-Pazos JM, Suarez J, et al. Tuberculous pleurisy: a study of 254 patients. Arch Intern Med. 1998;158(18):2017-2021.
doi pubmed - Cruz AT, Ong LT, Starke JR. Childhood pleural tuberculosis: a review of 45 cases. Pediatr Infect Dis J. 2009;28(11):981-984.
doi pubmed - Chiu CY, Wu JH, Wong KS. Clinical spectrum of tuberculous pleural effusion in children. Pediatr Int. 2007;49(3):359-362.
doi pubmed - Nance KV, Shermer RW, Askin FB. Diagnostic efficacy of pleural biopsy as compared with that of pleural fluid examination. Mod Pathol. 1991;4(3):320-324.
- Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, Hirsch E, et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):512-521.
doi pubmed - Kelley SA, Kossoff EH. Doose syndrome (myoclonic-astatic epilepsy): 40 years of progress. Dev Med Child Neurol. 2010;52(11):988-993.
doi pubmed - Hinokuma N, Nakashima M, Asai H, Nakamura K, Akaboshi S, Fukuoka M, Togawa M, et al. Clinical and genetic characteristics of patients with Doose syndrome. Epilepsia Open. 2020;5(3):442-450.
doi pubmed - Singh A, Prabha R, Ahmad N, Chacham S, Mohan K, Gaurav K. A two-year-old male child with Doose syndrome: An unusual entity. Case Rep Int 2020;9:100077Z06AS2020.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
International Journal of Clinical Pediatrics is published by Elmer Press Inc.
