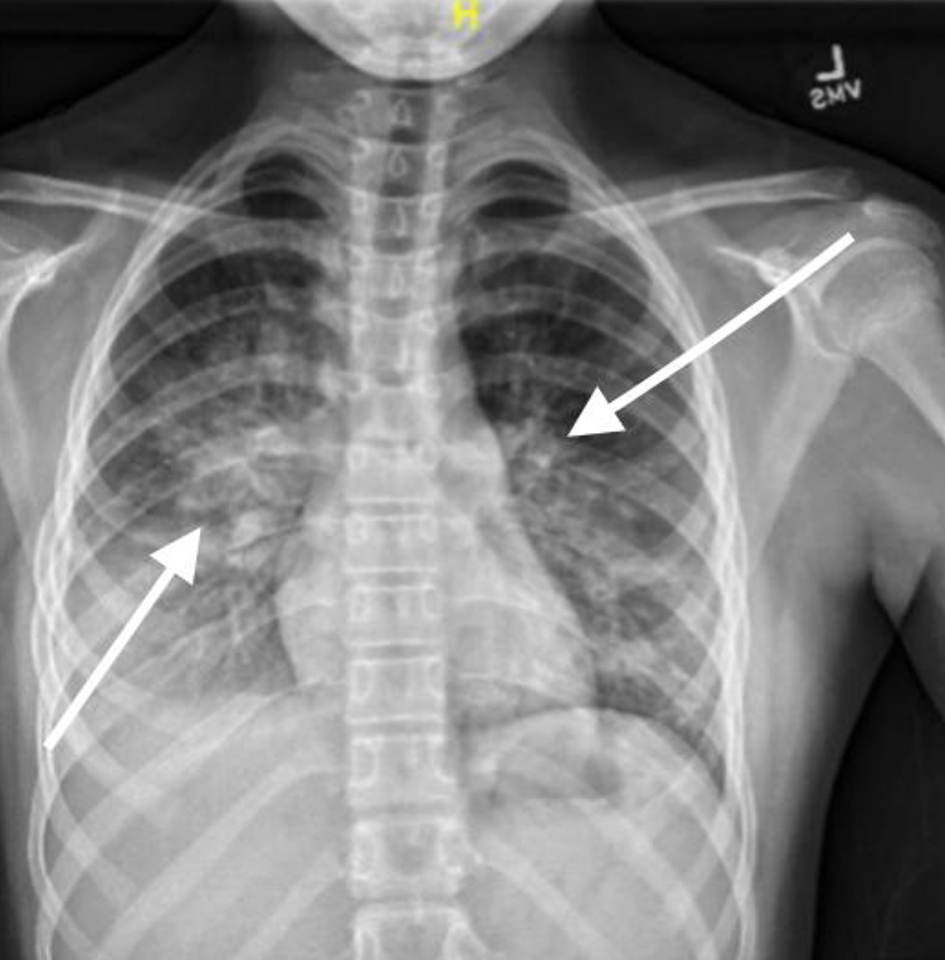
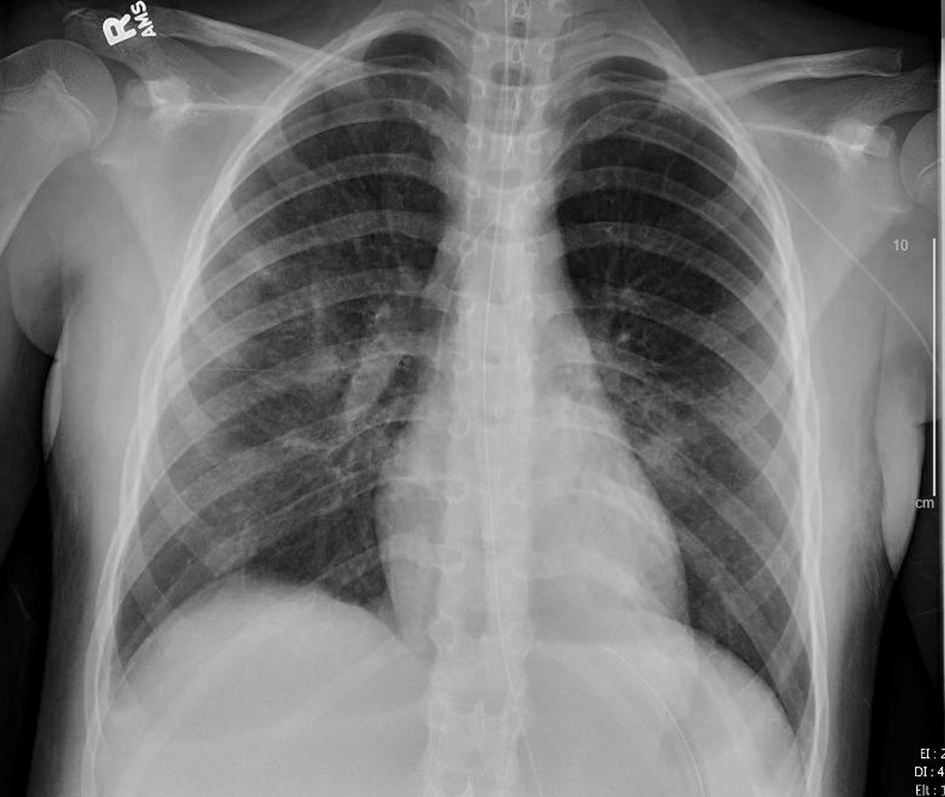
Figure 1. Chest X-ray, anteroposterior (AP) view on third presentation to emergency department showing signs of pneumonia with consolidation.
| International Journal of Clinical Pediatrics, ISSN 1927-1255 print, 1927-1263 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, Int J Clin Pediatr and Elmer Press Inc |
| Journal website http://www.theijcp.org |
Case Report
Volume 9, Number 2, June 2020, pages 41-49
SARS-CoV-2 in a Pediatric Patient Requiring Mechanical Ventilation and Multi-Drug Therapy
Figures


Tables
| Blood pressure (mm Hg) | - |
| Heart rate (beats per minute) | 139 |
| Respiratory rate (breaths per minute) | 20 |
| Temperature (°C) | 39.6 |
| Pulse Ox (%) | 100% on room air |
| Weight (kg) | 61 |
| Constitutional | Active, no acute distress, alert, well hydrated |
| Head/ears/nose/throat | Bilateral tympanic membranes are normal without erythema or bulging. Oral mucosa is moist. |
| Eyes | Conjunctivae normal. Pupils are equal, round and reactive to light. |
| Neck | Musculoskeletal: normal range of motion and neck supple. |
| Cardiovascular | Rate and rhythm: normal rate and regular rhythm. Heart sounds: S1 normal and S2 normal. |
| Pulmonary | Pulmonary effort is normal. No respiratory distress or retractions. Normal breath sounds and air entry. No decreased air movement. No wheezing. |
| Abdominal | Bowel sounds are normal. There is no distension. Abdomen is soft and flat. There is no abdominal tenderness, guarding or rebound. No right lower quadrant tenderness. Able to hop, smiles while hopping. |
| Integumentary | Skin is warm and dry. Capillary refill takes less than 2 s. No petechiae or rash, purpura or mottling. |
| Neurological | Patient is alert with no focal neurologic deficits. |
| Blood pressure (mm Hg) | 116/79 |
| Heart rate (beats per minute) | 137 |
| Respiratory rate (breaths per minute) | 16 |
| Temperature (°C) | 39.5 |
| Pulse Ox (%) | 96% on room air |
| Weight (kg) | 61 |
| Constitutional | Active, in no acute distress. She is well-developed and well-groomed. She is not toxic-appearing. |
| Head/ears/nose/throat | Normocephalic and atraumatic. Right ear: tympanic membrane, ear canal and external ear normal. Left ear: tympanic membrane, ear canal and external ear normal. Nose: no congestion or rhinorrhea. Mouth: mucous membranes are moist. Pharynx: uvula midline. Pharyngeal swelling and posterior oropharyngeal erythema present. No oropharyngeal exudate or pharyngeal petechiae. Tonsils: 2+ on the right, 2+ on the left. |
| Eyes | General: visual tracking is normal. Lids are normal. Vision grossly intact. Right eye: no discharge. Left eye: no discharge. Conjunctiva/sclera: conjunctivae normal. Pupils: pupils are equal, round and reactive to light. |
| Neck | Full passive range of motion without pain, normal range of motion and neck supple. Normal range of motion. No neck rigidity or pain with movement. |
| Cardiovascular | Rate and rhythm: normal rate and regular rhythm. Pulses: normal pulses. Pulses are strong. Heart sounds: S1 normal and S2 normal. No murmur. |
| Pulmonary | Pulmonary effort is normal. No respiratory distress. Normal breath sounds. No stridor, decreased air movement or transmitted. |
| Abdominal | Bowel sounds are normal. There is no distension. Abdomen is soft. Abdomen is not rigid. There is no mass. There is no abdominal tenderness. There is no right costovertebral angle (CVA) tenderness, no left CVA tenderness, guarding or rebound. |
| Lymphadenopathy | Cervical: cervical adenopathy present. Right cervical: superficial cervical adenopathy present. Left cervical: superficial cervical adenopathy present. |
| Integumentary | General: skin is warm and moist. Capillary refill: capillary refill takes less than 2 s. |
| Neurological | Mental status: she is alert and oriented for age. Glasgow coma scale (GCS): eye subscore: 4. Verbal subscore: 5. Motor subscore: 6. No cranial nerve deficit. No sensory deficit. |
| Test | Result | Reference range |
|---|---|---|
| aGrossly hemolyzed. | ||
| Sodium | 135 | 134 - 143 mmol/L |
| Potassium | 6.5a | 3.4 - 5.1 mmol/L |
| Chloride | 108 | 98 - 108 mmol/L |
| CO2 | 21 | 21 - 31 mmol/L |
| Blood urea nitrogen | 12 | 5 - 22 mg/dL |
| Creatinine | 0.53 | 0.30 - 0.80 mg/dL |
| Glucose | 88 | 70 - 110 mg/dL |
| Calcium | 8.4 | 8.9 - 10.4 mg/dL |
| Anion gap | 12.5 | 5.0 - 18.0 mEq/L |
| Red cell distribution width | 13.1 | 11.5-14.5% |
| Streptococcus pyogenes group A PCr throat | Negative | Negative |
| Urinalysis | Specific gravity 1.032 Glu neg Bili neg Ketone trace Blood 3+ Protein 100 Nitrite neg Leukocyte esterase neg Urine red blood cell 193 Urine white blood cell 4 Urine bacteria 2+ Urine mucus 1+ Squamous epithelial cells 17 | 1.002 - 1.030 Negative Negative Negative Negative < 20 mg/dL Negative Negative 0 - 5/HPF 0 - 9/HPF None None 0/HPF |
| Urine culture | No growth | |
| Blood pressure (mm Hg) | 90/71 |
| Heart rate (beats per minute) | 129 |
| Respiratory rate (breaths per minute) | 26 - 35 |
| Temperature (°C) | 39.6 |
| Pulse Ox (%) | 89% on room air |
| Constitutional | Active. Not in acute distress. Non-toxic-appearing. Able to speak in full sentences. |
| Head/ears/nose/throat | Normocephalic and atraumatic. Right and left external ear normal. No congestion or rhinorrhea. Mucous membranes are moist. No oropharyngeal exudate or posterior oropharyngeal erythema. |
| Eyes | Right eye: no discharge. Left eye: no discharge. Extraocular movements intact. Conjunctiva/sclera: conjunctivae normal. |
| Neck | Normal range of motion and neck supple. |
| Cardiovascular | Regular rhythm. Tachycardia present. Pulses: normal pulses. Normal heart sounds. |
| Pulmonary | Tachypnea and respiratory distress present. No nasal flaring or retractions. |
| Abdominal | Abdomen is flat. Bowel sounds are normal. There is no distension or tenderness to palpation. |
| Lymphadenopathy | No cervical lymphadenopathy appreciated on exam. |
| Integumentary | Skin is warm and dry. Capillary refill takes 2 - 3 s. |
| Neurological | No focal deficit present. She is alert and oriented × 4. Mood normal. Thought content normal. Judgment normal. |
| White blood cell | 5.47 | 4.5 - 13.5 × 103/µL |
| Red blood cell | 4.43 | 3.80 - 5.00 × 106/UL |
| Hemoglobin | 12.3 | 12.0 - 16.0 g/dL |
| Hematocrit | 35.4 (L) | 37.0-45.0% |
| Mean corpuscular volume | 79.8 | 78.0 - 102.0 fL |
| Mean corpuscular hemoglobin | 27.7 | 26.0 - 32.0 pg |
| Mean corpuscular hemoglobin concentration | 34.8 | 31.0-37.0% |
| Red cell distribution width | 13.1 | 11.5-14.5% |
| Platelet count | < 10 (LL) | 150 - 450 × 103/µL |
| Mean platelet volume | 15.1 (H) | 7.5 - 9.3 fL |
| Automated absolute neutrophil | 4.60 | 1.80 - 7.97 × 103/µL |
| Band | 13.0 (H) | 0-11% |
| Segmented neutrophils | 70.0 (H) | 40.0-59.0% |
| Lymphocyte | 13.0 (L) | 33.0-48.0% |
| Monocyte | 4.0 | 0.0-6.0% |
| Absolute neutrophil manual | 4.54 | 1.80 - 7.97 × 103/µL |
| Red blood cell morphology | Normal | |
| C-reactive protein | 11.5 | |
| Urinalysis | Specific gravity 1.009 Glu neg Bili neg Ketone 1+ Blood 3+ Nitrite neg Leukocyte esterase neg Urine red blood cell 14 Urine white blood cell 2 | |
| Urine culture | No growth | |
| Respiratory viral panel (RVP) | Negative | Ref range |
| Adenovirus PCr | Negative | Negative |
| Coronavirus 229E PCr | Negative | Negative |
| Coronavirus HKU1 PCr | Negative | Negative |
| Coronavirus NL63 PCr | Negative | Negative |
| Coronavirus OC43 PCr | Negative | Negative |
| HMPV PCr | Negative | Negative |
| Rhinovirus/enterovirus PCr | Negative | Negative |
| Influenza A PCr | Negative | Negative |
| Influenza B PCr | Negative | Negative |
| Parainfluenza 1 PCr | Negative | Negative |
| Parainfluenza 2 PCr | Negative | Negative |
| Parainfluenza 3 PCr | Negative | Negative |
| Parainfluenza 4 PCr | Negative | Negative |
| RSV PCr | Negative | Negative |
| Chlamydia pneumoniae PCr | Negative | Negative |
| Mycoplasma pneumoniae PCr | Negative | Negative |
| Therapy | Dosage | Route of administration | Frequency | Duration of treatment | Days received |
|---|---|---|---|---|---|
| IV: intravenous; HD: hospital day; PRN: as needed. | |||||
| Ceftriaxone | 2 g | IV | Daily | 7 days | Admission - HD 3 |
| Ampicillin | 2 g | IV | Daily | 1 day | Admission - HD 1 |
| Albuterol | 2.5 g | Inhaled nebulizer therapy | Every 3 h PRN | 14 days | Admission - HD 17 |
| Vancomycin | 20 mg/kg | IV | Every 8 h | 5 days | HD 2 - 6 |
| Cefepime | 2 g | IV | Every 8 h | 7 days | HD 3 - 10 |
| Azithromycin | 10 mg/kg | IV | Daily | 2 days | HD 3 - 4 |
| Azithromycin | 5 mg/kg | IV | Daily | 3 days | HD 5 - 7 |
| Tocilizumab | 600 mg | IV | Daily | 1 day | HD 7 |
| Tocilizumab | 600 mg | IV | Every 12 h | 1 day | HD 8 |
| Hydroxychloroquine | 400 mg | IV | Twice daily | 3 days | HD 6 - 8 |
| Clindamycin | 10 mg/kg | IV | Every 8 h | 3 days | HD 7 - 9 |
| Remdesivir | 200 mg | IV | Daily | 1 day | HD 8 |
| Remdesivir | 100 mg | IV | Daily | 9 day | HD 9 - 17 |