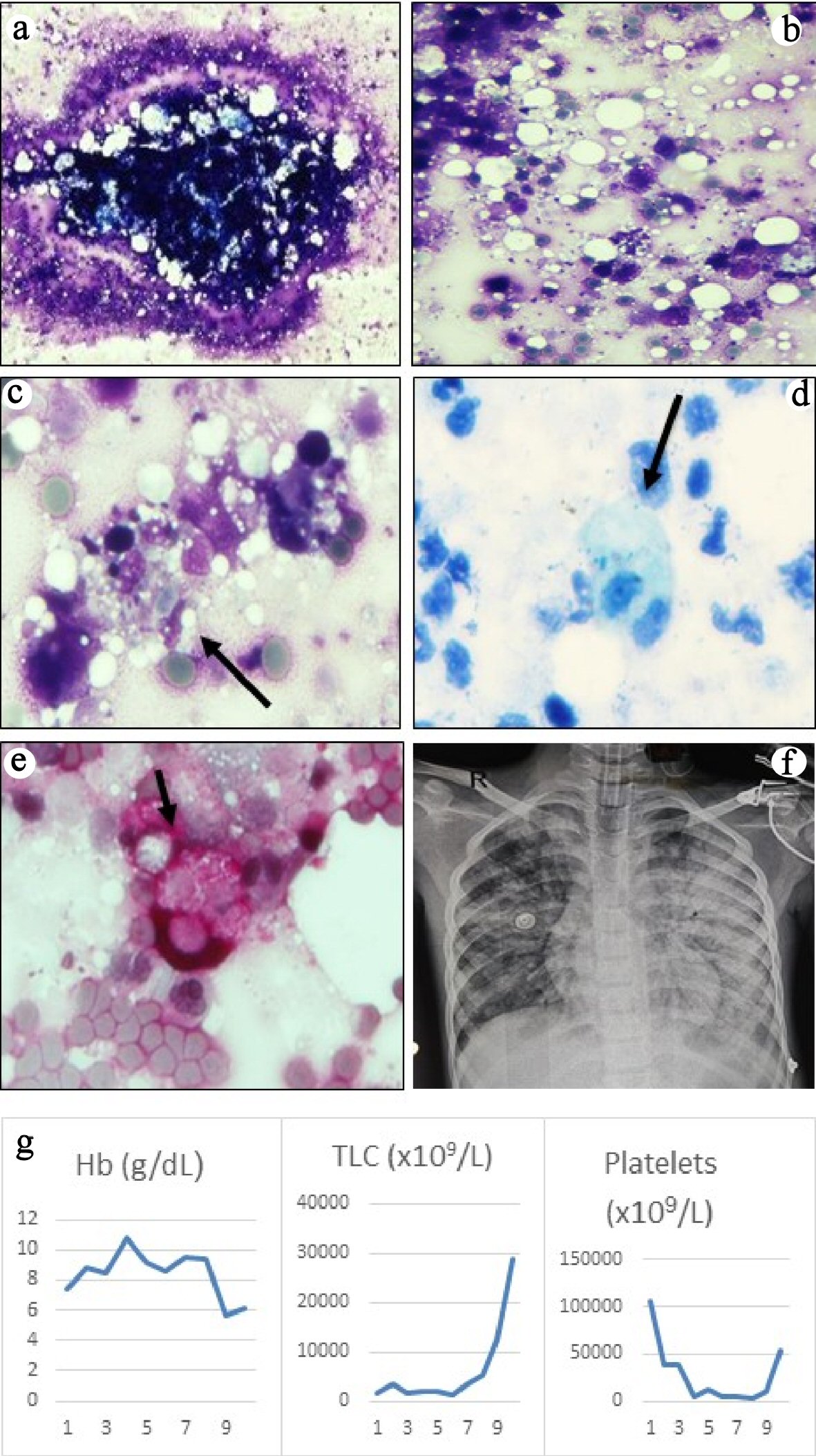
Figure 1. (a) Bone marrow aspirate smears were particulate and appeared normocellular (May-Grunwald Giemsa, × 40). (b) The background showed mostly necrotic cells with ill-defined cellular boundaries admixed with fat and very few viable cells (May-Grunwald Giemsa, × 200). (c) High power examination revealed several histiocytes with ingested erythrocytes, lymphocytes and cell debris (May-Grunwald Giemsa, × 400). Ziehl-Neelsen (ZN) stain for acid-fast bacilli (d) and periodic acid-Schiff stain for fungi (e) were negative, but highlighted the phagocytic histiocytes (× 400, ZN stain counterstained with methylene blue, PAS stain counterstained with hematoxylin). (f) Chest radiograph showed bilateral pulmonary edema secondary to transfusion-related lung injury. (g) Graphs showing trends of the blood counts during hospital stay.